-
PDF
- Split View
-
Views
-
Cite
Cite
Schauki Mahmoud, Amjad Soltany, A rare case report of gastro-duodenal fourth segment fistula secondary to a penetrating benign gastric ulcer, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz096, https://doi.org/10.1093/jscr/rjz096
Close - Share Icon Share
Abstract
A gastro-duodenal fourth segment fistula following a penetrating benign gastric ulcer is extremely rare to be found. To the best of our knowledge, our case is the eighth case to describe the gastro-duodenal third and fourth segment fistula, and it is the third to be diagnosed in living patients as all the other cases were diagnosed in autopsies. The case, we are presenting, is of an elderly patient with severe peptic symptoms and a primary diagnosis of gastric outlet obstruction. During our indicated surgery, we accidently diagnosed this rare type of fistula. In the following article, we will describe the clinical features of this fistula, discuss the steps of our unique surgical management, and summarize our follow-up for the patient.
INTRODUCTION
Gastro-duodenal fistula describes a direct anatomical connection between the stomach and the duodenum. These fistulas following certain conditions like carcinoma, Crohn’s disease and lymphoma are well described in medical literature [1]. On the other hand, these secondary to benign gastric ulcer are relatively uncommon. These fistulas could be asymptomatic or of obvious peptic symptoms [2, 3]. Treatment of these fistulas depends mainly on the severity of patient’s symptoms [3, 4].
CASE REPORT
A 61-year-old man was presented to our department with epigastric discomfort, general weakness, weight loss (~14 kg in 4 months), constipation, melena and vomiting for the last 4 months of solid intake 1 h after each meal. There was a good tolerance to liquid intake.
Physical examination revealed that the patient was afebrile, slightly pale, hemodynamically stable with no jaundice. We noticed an abdominal scar of midline incision and a mild tenderness in epigastrium. No organomegaly was found.
Previously, 1 month ago, the patient was admitted for the same complaints. He underwent upper gastrointestinal endoscopy which was unsuccessful because of the residual food in his stomach. The patient was put on omeprazole 20 mg twice daily with a re-evaluation after a month.
The patient’s past surgical history included perforated benign first portion of duodenal ulcer 15 years ago (treated by primary closure and graham patch) and cholecystoctomy with no other significant medical history.
Admission work-up is shown in Table 1.
| White blood cell count | Hemoglobin | Platelet | Glucose | Urea | Creatinine | Potassium | Sodium |
| 5900 mm3 | 9.2 g/dL | 26 3000 mm3 | 78 mg/dL | 31 mg/dL | 1.31 mg/dL | 3.6 mmol/L | 137 mmol/L |
| Total protein | Albumin | Total bilirubin | Direct bilirubin | Alanine aminotransferase | Amylase | ||
| 6.8 g/dL | 3.5 g/dL | 0.6 mg/dL | 0.2 mg/dL | 25 U/L | 100 U/L |
| White blood cell count | Hemoglobin | Platelet | Glucose | Urea | Creatinine | Potassium | Sodium |
| 5900 mm3 | 9.2 g/dL | 26 3000 mm3 | 78 mg/dL | 31 mg/dL | 1.31 mg/dL | 3.6 mmol/L | 137 mmol/L |
| Total protein | Albumin | Total bilirubin | Direct bilirubin | Alanine aminotransferase | Amylase | ||
| 6.8 g/dL | 3.5 g/dL | 0.6 mg/dL | 0.2 mg/dL | 25 U/L | 100 U/L |
| White blood cell count | Hemoglobin | Platelet | Glucose | Urea | Creatinine | Potassium | Sodium |
| 5900 mm3 | 9.2 g/dL | 26 3000 mm3 | 78 mg/dL | 31 mg/dL | 1.31 mg/dL | 3.6 mmol/L | 137 mmol/L |
| Total protein | Albumin | Total bilirubin | Direct bilirubin | Alanine aminotransferase | Amylase | ||
| 6.8 g/dL | 3.5 g/dL | 0.6 mg/dL | 0.2 mg/dL | 25 U/L | 100 U/L |
| White blood cell count | Hemoglobin | Platelet | Glucose | Urea | Creatinine | Potassium | Sodium |
| 5900 mm3 | 9.2 g/dL | 26 3000 mm3 | 78 mg/dL | 31 mg/dL | 1.31 mg/dL | 3.6 mmol/L | 137 mmol/L |
| Total protein | Albumin | Total bilirubin | Direct bilirubin | Alanine aminotransferase | Amylase | ||
| 6.8 g/dL | 3.5 g/dL | 0.6 mg/dL | 0.2 mg/dL | 25 U/L | 100 U/L |
An upper gastrointestinal endoscopy was performed again after having the patient fast overnight with these findings (Fig. 1): residual food in stomach, pyloric edema and severe stenosis of the bulb that prevented us from progressing further into the small intestine. Biopsies were taken from the bulb and the atrophic mucosa of antrum. Histopathology revealed mild chronic atrophic gastritis and non-specific chronic duodenitis with no findings of either helicobacter pylori infection or malignancy. Colonoscopy, on the other hand, was within normal.

An upper gastrointestinal endoscopy shows pyloric edema and severe stenosis of the bulb.
Intravenous contrast computed tomography showed thickening of proximal gastric and pyloric walls and a mild dilatation of extra- and intra-hepatic bile ducts, although the head of pancreas was normal (Fig. 2).
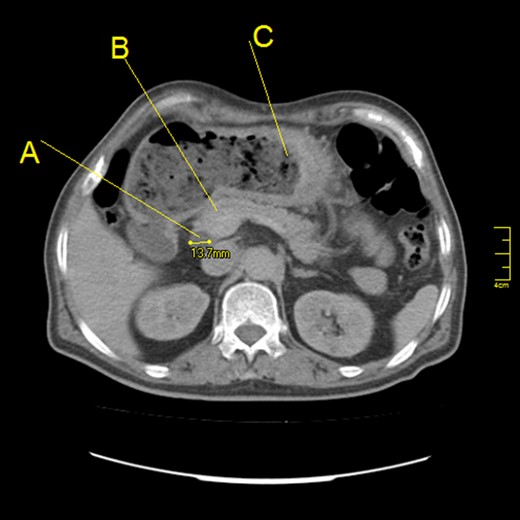
Abdominal computed tomography scan (axial section) showing: (A) Dilatation of common bile duct (a diameter of 13.7 mm). (B) Normal head of pancreas. (C) Thickening of greater curvature with a high amount of residual food.
The primary diagnosis was gastric outlet obstruction due to a complicated benign duodenal ulcer. The diagnosis was based on the benign endoscopic histopathology findings of the bulb and the rarity of duodenal malignancy. The decision then was to perform elective laparotomy because of both refractory symptoms despite of medical treatment with proton pump inhibitors and the lack of medical experience in endoscopic dilation in the hospital. During surgery, we found severe adhesions caused by the previous surgery which required careful adhesiolysis. The stomach was dilated and thick-walled. A stenosis of duodenal bulb was also detected. Surprisingly, we palpated a mass (5 × 7 cm) arising from the posterior lower half of greater curvature extending to the lesser sac. Anatomically, this mass (Fig. 3) represents a gastro-duodenal fourth segment fistula.
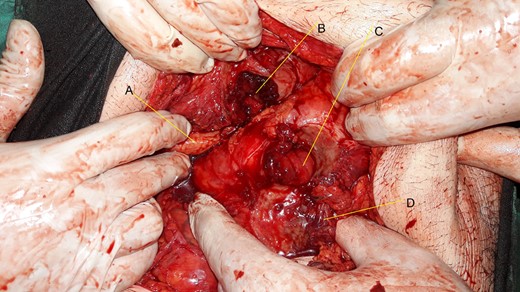
(A) Body of pancreas. (B) Perforated ulcer (3 by 3 cm) in the lower half of the posterior wall of the greater curvature with clear fibrosis. (C) A perforation (3 by 3 cm) in the top of the fourth portion of the duodenum. (D) Mesentery of transverse colon.
The surgical steps were (Fig. 4): Antrectomy, resection of the fourth duodenum, end to end third duodenojejunostomy, Omega-Braun gastrojejunostomy, feeding jejunostomy and drainage. Histopathology study revealed a perforated benign gastric ulcer (Fig. 5).
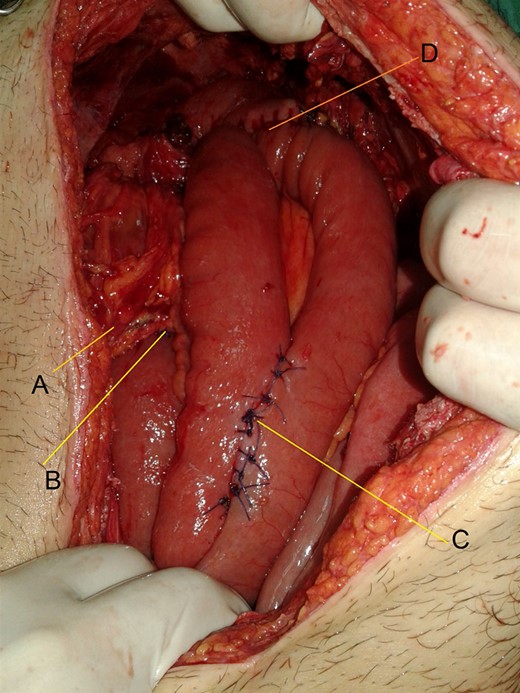
(A) Superior mesenteric vessels. (B) End to end third duodenojejunostomy. (C) Braun anastomosis. (D) Gastrojejunostomy.
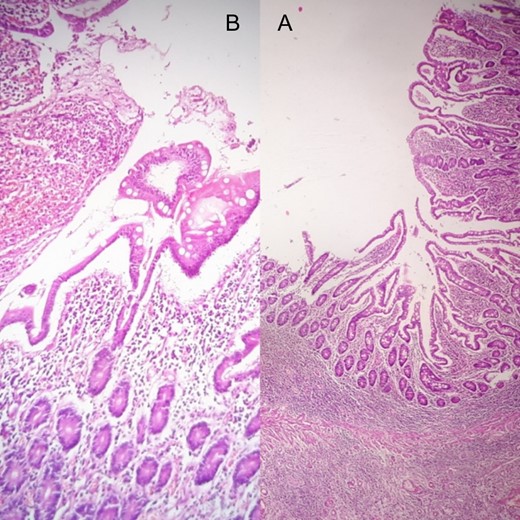
Both of (A) biopsy from the fourth duodenal segment and (B) biopsy from the greater curvature of stomach reveal a perforated benign gastric ulcer.
With a strict post-operative follow-up (shown in Table 2) for the patient, he was discharged home in 9 days.
| Post operation . | Follow-up . |
|---|---|
| On the first day | -Low urine output |
| -Work-up: urea: 70 mg/dL, creatinine: 1.8 mg/dL,glucose :200 mg/dL, total protein: 4.5 g/dL, albumin: 2.7 g/dL, hemoglobin: 10 g/dL | |
| - Good hydration plus human albumin intravenous were administrated | |
| On the second day | -Water feeding per jejunostomy tube |
| -Improvement of both urine output and renal function test | |
| On the third day | -Active bowel sounds |
| -Start of liquid diet feeding per jejunostomy tube with good tolerance | |
| On the fourth day | -The patient passed stool |
| -Work-up: albumin: 4 g/dL, total protein: 5.6 g/dL, hemoglobin: 10.2 g/dL | |
| On the fifth day | -Left sub-diaphragmatic and pelvis drains were removed |
| -Good wound healing | |
| On the seventh day | -Start of liquid oral feeding |
| On the ninth day | -Remaining drains were removed and the patient discharged home on (Omeprazole 40 mg once daily plus vitamin B12 1000 µg intramuscular monthly) |
| On the 15th day | -Removal of feeding jejunostomy tube |
| After 3 months | -No peptic symptoms |
| -Weight gain (~6 kg during these 3 months) |
| Post operation . | Follow-up . |
|---|---|
| On the first day | -Low urine output |
| -Work-up: urea: 70 mg/dL, creatinine: 1.8 mg/dL,glucose :200 mg/dL, total protein: 4.5 g/dL, albumin: 2.7 g/dL, hemoglobin: 10 g/dL | |
| - Good hydration plus human albumin intravenous were administrated | |
| On the second day | -Water feeding per jejunostomy tube |
| -Improvement of both urine output and renal function test | |
| On the third day | -Active bowel sounds |
| -Start of liquid diet feeding per jejunostomy tube with good tolerance | |
| On the fourth day | -The patient passed stool |
| -Work-up: albumin: 4 g/dL, total protein: 5.6 g/dL, hemoglobin: 10.2 g/dL | |
| On the fifth day | -Left sub-diaphragmatic and pelvis drains were removed |
| -Good wound healing | |
| On the seventh day | -Start of liquid oral feeding |
| On the ninth day | -Remaining drains were removed and the patient discharged home on (Omeprazole 40 mg once daily plus vitamin B12 1000 µg intramuscular monthly) |
| On the 15th day | -Removal of feeding jejunostomy tube |
| After 3 months | -No peptic symptoms |
| -Weight gain (~6 kg during these 3 months) |
| Post operation . | Follow-up . |
|---|---|
| On the first day | -Low urine output |
| -Work-up: urea: 70 mg/dL, creatinine: 1.8 mg/dL,glucose :200 mg/dL, total protein: 4.5 g/dL, albumin: 2.7 g/dL, hemoglobin: 10 g/dL | |
| - Good hydration plus human albumin intravenous were administrated | |
| On the second day | -Water feeding per jejunostomy tube |
| -Improvement of both urine output and renal function test | |
| On the third day | -Active bowel sounds |
| -Start of liquid diet feeding per jejunostomy tube with good tolerance | |
| On the fourth day | -The patient passed stool |
| -Work-up: albumin: 4 g/dL, total protein: 5.6 g/dL, hemoglobin: 10.2 g/dL | |
| On the fifth day | -Left sub-diaphragmatic and pelvis drains were removed |
| -Good wound healing | |
| On the seventh day | -Start of liquid oral feeding |
| On the ninth day | -Remaining drains were removed and the patient discharged home on (Omeprazole 40 mg once daily plus vitamin B12 1000 µg intramuscular monthly) |
| On the 15th day | -Removal of feeding jejunostomy tube |
| After 3 months | -No peptic symptoms |
| -Weight gain (~6 kg during these 3 months) |
| Post operation . | Follow-up . |
|---|---|
| On the first day | -Low urine output |
| -Work-up: urea: 70 mg/dL, creatinine: 1.8 mg/dL,glucose :200 mg/dL, total protein: 4.5 g/dL, albumin: 2.7 g/dL, hemoglobin: 10 g/dL | |
| - Good hydration plus human albumin intravenous were administrated | |
| On the second day | -Water feeding per jejunostomy tube |
| -Improvement of both urine output and renal function test | |
| On the third day | -Active bowel sounds |
| -Start of liquid diet feeding per jejunostomy tube with good tolerance | |
| On the fourth day | -The patient passed stool |
| -Work-up: albumin: 4 g/dL, total protein: 5.6 g/dL, hemoglobin: 10.2 g/dL | |
| On the fifth day | -Left sub-diaphragmatic and pelvis drains were removed |
| -Good wound healing | |
| On the seventh day | -Start of liquid oral feeding |
| On the ninth day | -Remaining drains were removed and the patient discharged home on (Omeprazole 40 mg once daily plus vitamin B12 1000 µg intramuscular monthly) |
| On the 15th day | -Removal of feeding jejunostomy tube |
| After 3 months | -No peptic symptoms |
| -Weight gain (~6 kg during these 3 months) |
DISCUSSION
In the medical literature, there are two types of gastro-duodenal fistulas. Both could be a complication of benign gastric ulcer.
Type I (double pyloric) joins lesser curvature and antrum to the first part of duodenum. Type II, which is extremely less common, joins the posterior wall and greater curvature of stomach to the third or fourth part of duodenum, and commonly involves the pancreas in its structure just like our case [4]. Because lesser curvature is considered the most common position for gastric ulcers [5], type I could by seen more frequently.
In general, fistulas following benign gastric ulcers could join stomach with colon, small intense, gallbladder, pleural cavity and pericardium [6].
The patient’s anemia was caused by chronic hemorrhage of the ulcer in addition to the malnutrition secondary to prolonged vomiting following the stenosis of bulb. However, the patient’s electrolytes were within normal, due to the fistula which played a role as an anatomical passage for fluids not for solid food. Type II seems to accompany with gastric outlet obstruction [4] which may be the cause of accumulation of gastric acid in the greater curvature and this could tiger the incidence of gastric ulcer there. In our case, the chronic ulcer had entirely eroded the gastric posterior wall, the pancreatic portion and the top of the adjacent fourth portion of the duodenum, consequently forming this mass.
Symptoms of these fistulas, which may vary among patients, include abdominal pain, nausea, discomfort, melena, weight loss, in addition to wide possibilities of peptic symptoms [2].
These fistulas could be diagnosed by either radiography (fluoroscopy and contrast study) or upper gastrointestinal endoscopy [6]. Also, they may be diagnosed accidently during surgery. We could not make our diagnosis of the fistula based on the upper gastrointestinal endoscopy because of the residual food. Treatment should be based mainly on severity of symptoms.
Type I usually does not require surgery, because most of cases respond to medical therapy like proton pump inhibitors, so surgery should be reserved for refractory cases [3].
On the other hand, management of type II is not obvious like type I because of severe lack of this type of fistula, so treatment should be based on patient’s condition. In our case, the surgery was indicated because of gastric outlet obstruction and severity of patient’s symptoms.
The only described surgical management for type II was Billroth II with a simple closure of the duodenal side of fistula [4].
Regarding our unique surgical management, a resection of the fourth segment of duodenum was performed. Because of the lack of frozen section techniques in our hospital, we could not make sure whether the ulcer was malignant or benign. Moreover, the wide diameter of the fibrotic opening of the duodenal fistula makes the primary closure unsafe, in addition to, the chronic inflammation caused attraction of the mesenteric wall of the fourth portion of the duodenum to the anti-mesenteric wall, which caused stenosis of lumen of the fourth portion, in its turn causing back-pressure that leads to a mild dilatation of extra and intra hepatic bile ducts and difficulty of solid food passage.
CONCLUSION
Regrettably, the medical literature on our topic (gastro-duodenal fourth segment fistula) is rather restricted which leaves a space for evaluation of the precious indications for surgery. We suggest that surgery is indicated for this specific type of fistula in case of severe peptic symptoms, biliary obstruction secondary to back-pressure, biliary gastritis and suspicion of malignancy. On the other side, surgery is not indicated in either asymptomatic cases or accidently diagnosed ones.
CONFLICT OF INTEREST STATEMENT
None declared.



