-
PDF
- Split View
-
Views
-
Cite
Cite
N Jayakody, M Faoury, W Hellier, H Ismail-Koch, S Patel, A Burgess, A rare presentation of a paediatric patient with acute otomastoiditis media caused by mycobacterium tuberculosis resulting in intracranial complications, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz093, https://doi.org/10.1093/jscr/rjz093
Close - Share Icon Share
Abstract
Mastoiditis caused by mycobacterium tuberculosis (TB) has an extremely low incidence in paediatric patients and intracranial complications are even rarer. We report the case of a 2-year-old Caucasian male who presented to a tertiary ENT centre with a left sided mastoid swelling and drowsiness after having been treated unsuccessfully for unresolving ear pain and discharge for 6 weeks. He was subsequently found to have mastoiditis with intracranial complications caused by mycobacterium TB. This report aims to increase awareness of TB as a potential cause of chronic unresolving ear pain in the paediatric age group, as well as the importance of multidisciplinary team management.
INTRODUCTION
Mycobacterium tuberculosis (TB) is an acid-fast bacillus that can manifest as either pulmonary or extra-pulmonary disease. Its incidence in UK has declined by 59% in the last 10 years down to 1.3 per 100 000 paediatric population in 2017 [1]. The middle ear mastoiditis as a primary site of infection caused by TB is extremely rare [2]. Only a handful of paediatric cases have been reported in the literature. We present the case of a 2-year-old male paediatric patient with otogenic tuberculosis and intracranial complications.
CASE REPORT
A 2-year-old Caucasian male presented to a tertiary care centre with a posterior auricular swelling and sudden deterioration with drowsiness and lethargy with a 6-week history of left-sided otalgia that he had been treated unsuccessfully with four courses of antibiotics/ear drops in primary care. He was noted to have a middle ear effusion and a temporo-auricular swelling more superior than expected from a subperiosteal mastoid collection.
A CT scan of the patient at this point showed mastoiditis, a subperiosteal abscess and extradural abscess with extensive bony defects (Figs 1 and 2). The patient was initially started on IV ceftriaxone and metronidazole. Upon discussion with ENT specialists he underwent a left sided mastoid exploration and drainage of the extradural and peri sigmoid sinus collection on Day 2 of his admission. Surgical exploration found a large parietal subperiosteal abscess with bony defects and granulation tissue connecting with an extradural abscess. Histological diagnosis showed evidence of granulomatous osteomyelitis due to necrotizing granulomatous inflammation. Initial Zeihl-Neelson and Wade Fire stains for acid fast bacilli in tissue culture were negative.
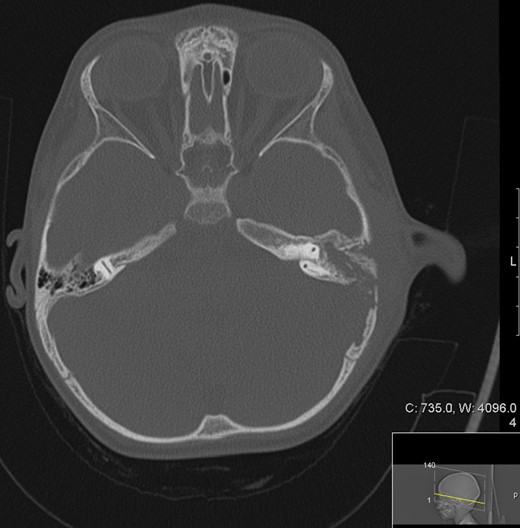
Transverse computed tomography (bone window) image showing a left sided mastoiditis (white asterisk) bone extensive cortical bony destruction involving left petrous, squamous and mastoid bone as well as the adjacent parietal bone.
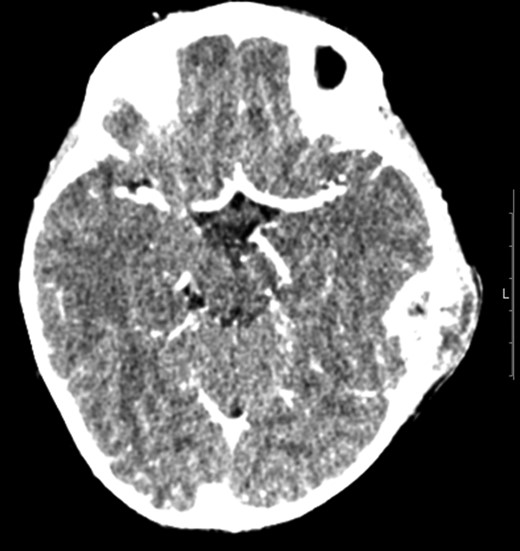
Transverse computer tomography with contrast (angiography), showing the extent of the extradural abscess (black asterisk). L = Left; R = Right. It shows that the left extracranial soft tissue abscess communicates freely through the parietal skull vault defect with the large intracranial extradural abscess, which spans the left tentorial leaflet.
Post-surgery, upon advice from the infectious diseases team, the patient was given 2 weeks of antibiotics (IV ceftriaxone and oral metronidazole) with a continuation of oral antibiotics (co-amoxiclav) for a further 4 weeks. This decision was based upon a real time PCR result positive for Group A streptococcus (cycle threshold value 45) from the surgical sample.
Patient underwent MRI imaging (Day 6 post drainage) which showed near resolution of the epidural and extracranial collection (Fig. 3). Upon review of images it was decided that no further surgical input was necessary, and the patient was discharged with follow up planned within 2 weeks.
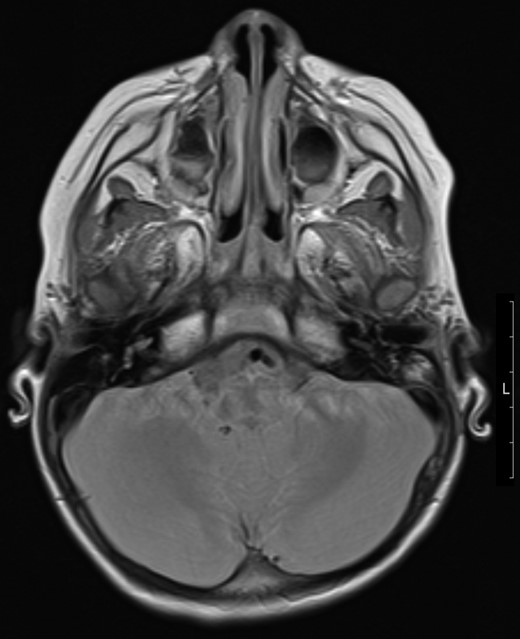
Transverse magnetic resonance image 3 months post op showing some residual inflammation within the post-surgical mastoid cavity (white asterisk) and resolution of collection.
The patient represented 2 weeks after with a recurring ear discomfort and agitation with ongoing left posterior auricular swelling. A repeat MRI scan showed reduction of the size of extradural collection and upon consultation between the ENT team and neurosurgeons no further surgical intervention was deemed necessary.
At this point, the mycobacterial culture (pus) was subsequently confirmed as fully sensitive mycobacterium TB. The patient was assessed for signs of disseminated TB, including a chest X-ray and lumbar puncture; both of which were negative. HIV serology was negative. The patient was started on Isoniazid OD (10 mg/kg), Rifampicin OD (15 mg/kg), Ethambutol OD (20 mg/kg) and pyrazinamide OD (35 mg/kg).
After consultation with the infectious disease team, it was decided that quadruple therapy for TB would continue for 2 months, followed by a further 10 months of dual therapy (rifampicin and isoniazid) plus pyridoxine. This was decided in line with TB in the central nervous system [3].
Although the patient was responding well to treatment, persistent lethargy and poor appetite resulted in a repeat MRI 3 months after he was initially started on anti-TB medication, which excluded an intracranial collection but revealed middle ear fluid which was subsequently drained by myringotomy and grommet insertion resulting in resolution of symptoms. The patient is currently responding well to therapy, with no clinical signs of recollection.
Screening for TB performed on close contacts including family proved negative. It subsequently transpired that an au-pair who had lived with the family for 12 months had been diagnosed with pulmonary TB after return to her native country.
DISCUSSION
Otogenic TB was first described by Jean Loius Petit [4]. Records from the early 20th century report an incidence of TB otitis media of 2.8% in the paediatric population by Fraser et al. (1915) [4]. The landscape has changed immensely since this time in line with the general reduction in TB associated with immunization programmes and socioeconomic factors such as improved housing [1]. Most sources are now associated with overseas contacts but even in TB endemic countries the occurrence of paediatric otogenic TB is rare with only a few paediatric case reports presented in literature (Fig. 4). Intracranial complications of otomastoiditis is even rarer and include meningitis, encephalitis, empyema, extradural collections and sinus venous thrombosis [5], which makes the management of such cases extremely challenging. And out of paediatric case reports presented, only one was found to have reported intracranial complications [6].
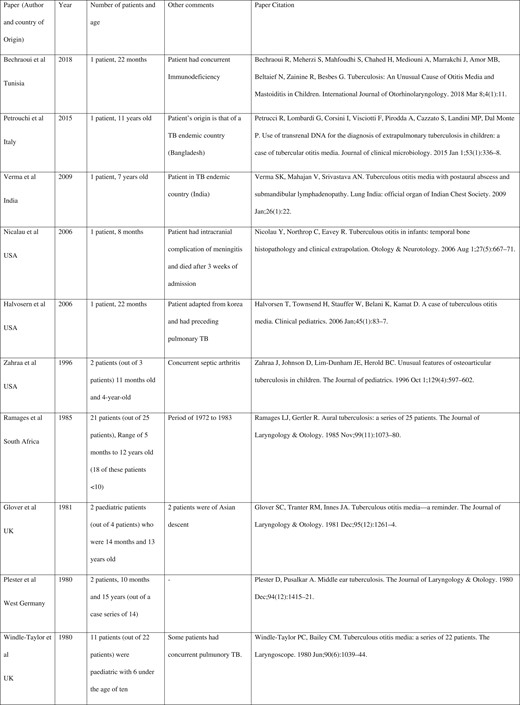
Literature overview of paediatric otomastoiditis case reports from 1980 onwards searched through OVID Medline and Embase databases and references of searched case reports. (With exclusion of non-English language-based case reports.)
Patients with TB otomastoiditis generally present with a range of non-specific symptoms such as otalgia, ear discharge, hearing loss and facial palsy [2, 7]. Signs included tympanic membrane perforation, aural polyps and granulation tissue formation [7] which overlap with many other infective causes which makes diagnosis of TB difficult.
The main investigations carried out are CT and MRI imaging for diagnostic and pre-surgical planning purposes [4, 6, 8]. There are no specific pathognomonic radiological signs for TB, although CT imaging in most of the case reports have shown destruction/erosions within the temporal bone [4, 6, 8]. Zeihl-neelson staining is the classical method of identifying TB whilst the typical histological description of TB is that of caseating granulomatous disease with Langerhans giant cells [4, 6]. Tests such as interferon gamma and TB PCR is increasingly used in current practice [9]. Management of neuro-otogenic TB includes involvement of multiple medical/surgical specialties. The involvement of infection experts is essential and most literature suggest long term anti-TB treatment including isoniazid, pyrazinamide, ethambutol for at least 2 months and isoniazid and rifampicin for 4 months [3]. Surgical management of the condition includes initial cortical mastoidectomy and intracranial drainage whilst more radical mastoidectomy for recurrent TB has been suggested in some studies [4, 6, 8]. Close follow up is advocated with repeated imaging depending on clinical progress.
This report aims to increase the awareness of TB as a potential rare source of neuro-otogenic infection in the paediatric population and the multidisciplinary approach to management involving quadruple medical therapy, surgery and ongoing clinical/radiological monitoring.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



