-
PDF
- Split View
-
Views
-
Cite
Cite
Duncan Henderson, James J P Alix, Saurabh Sinha, Holocord syrinx presenting with foot drop, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz082, https://doi.org/10.1093/jscr/rjz082
Close - Share Icon Share
Abstract
We present an unusual presentation of holocord syrinx. A 4-year-old boy presenting a 2-week history of right sided foot drop. An MRI revealed a holocord secondary to a chiari one malformation. He successfully underwent a craniocervical decompression. Post operatively the syrinx decreased in size and his foot drop completely resolved.
INTRODUCTION
Holocord syrinx is a recognised complication of chiari 1 malformation [1]. However, foot drop is a rare presenting complaint for this pathology. To our knowledge, there have been eight cases reported of holocord syrinx presenting as foot drop in the paediatric population [2–7].
CASE REPORT
A 4-year-old previously fit and well male presented with a 2-week history of a painless right sided foot drop. He was struggling to run and frequently falling. There was no history of developmental delay or trauma. He had no signs or symptoms of raised intra cranial pressure or sphincter disturbances. On clinical examination, ankle dorsiflexion was 1/5 on the right and there was diminished sensation in the right L5 dermatome. He was otherwise neurologically intact.
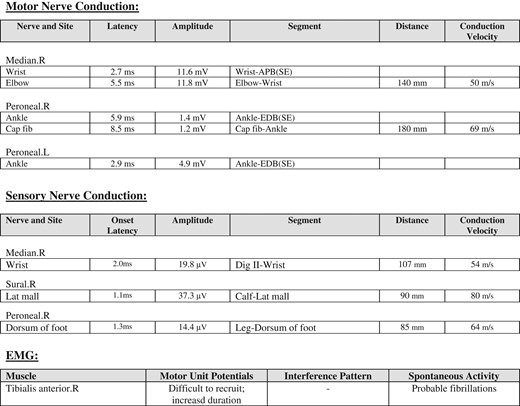
An MRI demonstrated a chiari one malformation (Fig. 1) with holocord syrinx (Fig. 2). No space occupying lesion was seen in the spine and the cord was not tethered. Neurophysiological investigations were carried out (Fig. 3), the child found the nerve conduction studies (NCS) and electromyography (EMG) difficult to tolerate however the findings were in keeping with pre-ganglionic pathology. There was evidence from the motor NCS and EMG of neurogenic abnormalities, including active denervation and re-innervation at the L4/5 level. These findings could have been at the level of the root or anterior horn. However, these findings were not considered typical for a peroneal neuropathy as the peroneal sensory potential was within normal limits.
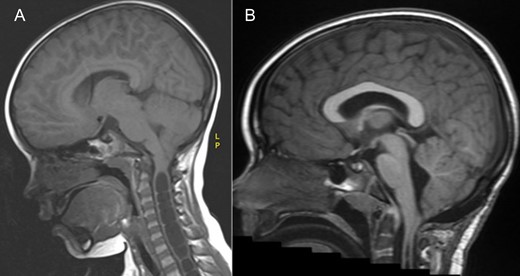
MRI brain demonstrating the chiari 1 malformation. Pre-op sagittal T1 showing cerebellar tonsillar descent of 9 mm below the foramen magnum (A) and at 3 years post op showing adequate hind brain decompression (B).
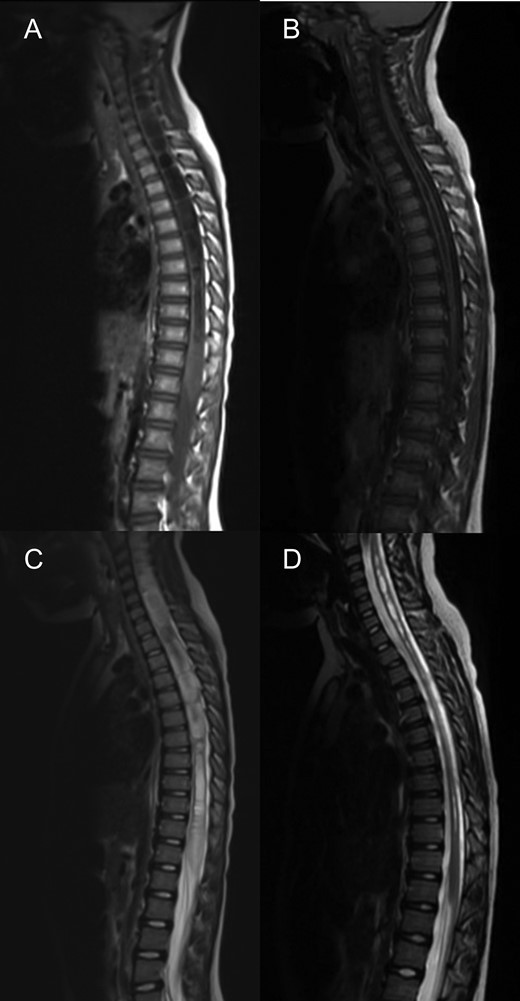
MRI spine sagittal sections demonstrating a holocord syrinx decreasing in size following surgery. Pre (A) and 3 years post op (B) T2. Pre (C) and 3 years post op (D) and T1.
A craniocervical decompression was performed. Intra-operative ultrasound demonstrated that there was no CSF flow at the level of the foramen magnum. Therefore the dura was opened, no duraplasty was used. There were no post-operative complications.
At 1 year follow-up, his foot drop had gradually improved. He was able to walk on his tip toes and heels. By 2 years follow-up, his foot drop had completely resolved and ankle dorsiflexion was 5/5 on the right. An MRI at three years post op demonstrated a good foramen magnum decompression (Fig. 1) and significant improvements in the syrinx (Fig. 2), however not complete resolution.
DISCUSSION
We present a case of a 4-year old boy with holocord syrinx secondary to chiari one malformation, presenting with a unilateral foot drop which completely resolved following a craniocervical decompression.
To our knowledge, there are eight other similar cases reported in the paediatric population. The ages ranged from 4 to 16 years old [2–7]. In the six patients managed operatively, all have experienced a significant improvement in their foot drop following surgery [3–6]. Of the other two reported cases, one patient was still awaiting a craniocervical decompression at the time of publication [7] and the other declined neurosurgical intervention [2].
In all cases managed operatively, a suboccipital craniectomy and C1 laminectomy were performed. In our case, we performed an intra-operative ultrasound and decided not to open the dura as good CSF flow was observed. However, other neurosurgeons have used both autologous and bovine duraplasty successfully [4, 6].
We observed a reduction in the syrinx volume, which was similar to the other cases described [3–6] however complete radiological resolution of the holocord syrinx has also been described [6].
CONFLICT OF INTEREST STATEMENT
None declared.



