-
PDF
- Split View
-
Views
-
Cite
Cite
Glenda Herrera C., Amílcar Herrera C., Patricia Pontón, Gabriel Alejandro Molina, Jonathan Eduardo Constante, Jhony Alejandro Delgado, Amebiasis, a rare cause of acute appendicitis, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz076, https://doi.org/10.1093/jscr/rjz076
Close - Share Icon Share
Abstract
Acute appendicitis is one of the most common abdominal emergencies, even though most cases of appendicitis will be due to obstruction of the appendiceal lumen, in rare occasions and mostly due to poor sanitary conditions a parasitic infection may cause appendicitis. Entamoeba histolytica is a common parasite and has a broad clinical spectrum from an asymptomatic disease to a life-threatening condition. In rare occasions, trophozoites can invade the appendiceal wall causing appendicitis. Preoperative diagnosis of acute amebic appendicitis is usually difficult, yet surgical treatment as in non-amebic appendicitis is the treatment of choice. However, due to the increased rate of postoperative complications associated with acute amebic appendicitis, a course of nitroimidazoles, and increased awareness in basic sanitary measures is usually recommended. We present a case of a 29-year-old woman, she presented with abdominal pain and appendicitis was suspected. After successful surgery, pathology confirmed acute amebic appendicitis.
INTRODUCTION
Appendectomy is one of the most common surgical procedures, many microorganisms have been associated with this disease, including bacteria and occasionally parasites [1, 2]. Entamoeba histolytica is the parasite responsible for amebiasis and infects up to 10% of the world’s population [2]. Appendicitis caused by E. histolytica is a rare phenomenon and care must be taken especially when regarding postoperative care as complication rates tend to be higher than non-amebic appendicitis [2, 3].
We present a case of a 29-year-old woman with acute amebic appendicitis who underwent complete recovery.
CASE REPORT
Patient is a 29-year-old woman without any past medical history, she presented to the emergency room with a 2-day history of abdominal pain and nausea, the pain first appeared on the epigastric region but in the last 12 hours the pain became more severe and migrated to the right lower quadrant. There were no accompanying symptoms such as dysuria or diarrhea. On clinical examination, a dehydrated and febrile patient was encountered, her abdomen was sensitive to gentle pressure and diffuse pain was discovered in her lower abdomen. Laboratory exams revealed mild leukocytosis with neutrophilia. Due to her condition and to rule out other surgical causes, a contrast-enhanced computed tomography (CT) revealed a distended cecum, a slight amount of free liquid in her abdomen and an inflamed appendix. The proximal third of the appendix measured more than 6 mm (Fig. 1A and B).
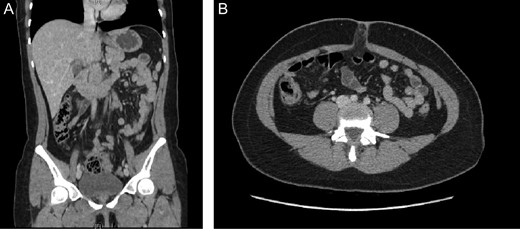
(A) Contrast-enhanced CT, revealing an inflamed appendix. (B) Contrast-enhanced CT, surrounded by heterogeneous inflamed fat.
Acute appendicitis was the suspected and a surgical assessment was required. After antibiotics were initiated, surgery was decided. At laparoscopy, the appendix was seen distended and had multiple inflammatory patches on its wall. Also, about 15cc of inflammatory liquid was seen in the pelvic cavity. An appendectomy was performed and the rest of the procedure was completed without any complications.
Pathology reported acute appendicitis due to amebiasis, scarce polymorphonuclear inflammatory infiltrate was seen in the mucosa accompanied by edema and congestion, also the presence of grown trophozoites of E. histolytica were seen in the appendicular lumen and wall. (Fig. 2A and B)
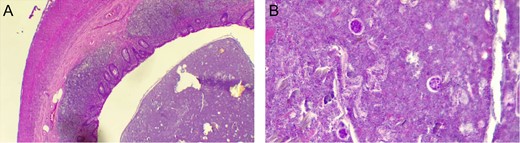
(A) Polymorphonuclear inflammatory infiltrate in the appendix wall. (B) Trophozoites of E. histolytica in the appendicular wall.
The postoperative course of this patient was uneventful, sips of liquids were initiated in the early postoperative period and after a course of metronidazole, she was discharged without complications. On follow-up controls, the patient is doing well.
DISCUSSION
Human infection with parasites has been recognized for thousands of years [1]. Amebiasis is the second leading cause of death from parasitic disease worldwide and occurs predominantly due to lack of sanitary-hygienic conditions [2, 3]. Due to its broad spectrum of behavior, it can present as an asymptomatic disease to a lethal condition with catastrophic events in the colon and liver [1, 2]. Entamoeba exists as two genetically distant species, Entamoeba dispar, a commensal, and E. histolytica, the pathogen. Diagnosis is based on the demonstration of Entameba in the stool or the colonic mucosa of the patients, serologic exams can also be performed [2]. Appendicitis is the most common cause of an acute surgical abdomen, with an estimated lifetime prevalence of 8%. Appendicitis is caused due to the obstruction of the appendiceal lumen, this may result from a variety of causes, which include fecaliths, lymphoid hyperplasia, foreign bodies, tumors, and parasites [4]. As it was found in our case.
Acute appendicitis due to E. histolytica is relatively rare with an incidence of 0.5–2.3% [5] There are no specific symptoms for acute amebic appendicitis and cannot be clinically differentiated from non-amebic appendicitis [3]. Diagnosis is based on clinical findings as most patients will experience pain in the right lower abdominal quadrant, the coexistence of bloody diarrhea at the time of diagnosis is uncommon [6]. As we discovered in our patient.
One could suspect amebiasis if there is a history of traveling to a high-risk country nonetheless this information is regularly missed [2, 6]. Treatment is usually the same as non-amebic appendicitis, however, metronidazole treatment should be administered for at least 5 days, in all histopathologically confirmed cases, as the postoperative complication rate of acute amebic appendicitis is higher than non-amebic appendicitis cases [3, 7]. Although clinical management of acute amebic appendix has been described. Due to morbidity and mortality rates associated with acute amebic particularly when surgery is delayed and as appendectomy removes the focus of infection it should be considered the treatment of choice [2, 8]. As it was done in our patient.
Thorough knowledge of amebic pathology and its varied clinical presentations are needed for all surgeons, especially the ones that live in places with poor sanitary controls as our own. A high index of suspicion is needed when confronted with amebiasis as it can mimic many colonic diseases. As health care providers we must heighten the awareness of the importance of good hygiene habits education especially in areas that lack basic health services and access to drinking water.
CONFLICT OF INTEREST STATEMENT
None declared.



