-
PDF
- Split View
-
Views
-
Cite
Cite
Fabian Wehrmann, Elsheikh Hashim, Shahbaz Mansoor, Ingested partial denture mimicking perforated diverticular disease, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz071, https://doi.org/10.1093/jscr/rjz071
Close - Share Icon Share
Abstract
Denture ingestion is a rare clinical entity among foreign body ingestions. The caveat is that there is often no recollection of the event and that dentures are radiolucent and as such hard to identify on conventional imaging. To date not all dentures contain radiopaque marker. Here we present the case of a 52-year-old male who was admitted with clinical and radiological signs of perforated diverticular disease. A curvilinear metallic foreign body was picked up on repeat CT imaging at day 3, which was part of an unknowingly swallowed partial denture that became impacted and perforated the sigmoid colon. The patient underwent an uneventful laparoscopic anterior resection and was discharged home a week later. We conclude that all dentures should contain a radiopaque marker in order to avoid failure in radiological detection and thus prevent misdiagnosis and inappropriate treatment.
INTRODUCTION
Foreign body ingestion (FBI) is a common clinical entity encountered in A&E. Most foreign bodies pass the digestive tract freely, whereas 10–20% require an interventional procedure. In 1% of the cases it leads to intestinal perforation, usually at areas of acute angulation or luminal narrowing such as the terminal ileum, ileo-cecal valve or the colorectal region [1, 2]. The ingestion of dentures can lead to impaction and intestinal perforation with serious complications and even fatal outcome [3–5]. Complications occur often due to delay in the diagnosis. One reason is that the ingestion is often not recollected at the time of admission and additionally, dentures can be difficult to identify on conventional imaging. Here we present the case of a 52-year old male that was admitted with clinical and radiological features of perforated diverticular disease. The perforation was caused by an unknowingly swallowed partial denture, which was identified on follow-up CT imaging. After failed endoscopic removal, a laparoscopic anterior resection was performed, which contained the partial denture that perforated the wall of the sigmoid colon.
CASE REPORT
A 52-year male was referred to the surgical team for a 1-day history of left iliac fossa pain accompanied by nausea and the inability to open his bowels for 48 hours. The pain was 9/10 in severity, sharp, persistent and with a gradual worsening onset. The patient was previously diagnosed with extensive diverticular disease and admitted 2 months prior with acute sigmoid diverticulitis. 18 months earlier he underwent an emergent laparoscopy for an unclear pelvic inflammatory mass on CT, that suggested either severe sigmoid diverticulitis or appendicitis. He also had multiple polyps throughout the colon, that were endoscopically removed. The patients past medical history was significant for a non-flow limiting coronary artery disease, arterial hypertension and an allergy to penicillin and tetracycline. Temperature on admission was 38.7 C, blood pressure of 149/109 mm/Hg, pulse of 109 bpm and a respiratory rate of 20/min with O2-saturations of 96% on room air. The abdomen was soft with tenderness and guarding over the left iliac fossa. Bowel sounds were present. Investigations showed a white cell count of 17.6 tsd/ul and a CRP of 64 mg/l. No pneumoperitoneum was detected on an erect chest x-ray. Treatment with ciprofloxacin and metronidazole was started and the patient kept nil per mouth. CT imaging showed extensive sigmoid diverticular disease with marked pericolonic fat stranding and free gas tracking into the mesenteric fat. Gentamycin was added and within 3 days the patient’s clinical symptoms improved. He was apyrexic and the white cell count dropped to 10.9 tsd/ul. A repeat CT scan showed a stable appearing localized perforation with reduced free gas and no signs of collection. However, of note was a small curvilinear metallic foreign body within the lumen of the sigmoid colon of uncertain etiology (Fig. 1). On questioning, the patient recalled a mechanical fall with a head contusion 9 days prior to admission during which he lost his partial denture. The patient was commenced on laxatives and despite bowel movement on the following day, the foreign body did not pass. A PFA showed the persistent presence of the metallic foreign body over the sigmoid colon, which raised the suspicion of impaction (Fig. 2). The patient was prepared for colonoscopy and the foreign body was identified impacting the lumen of the sigmoid colon (Fig. 3). However, endoscopic retrieval failed and the decision was made to proceed with laparoscopic anterior resection. Intraoperative findings showed a rigid and thickened sigmoid colon with adhesions and a diverticular abscess. About 22 cm of sigmoid colon was resected and the procedure was completed with a primary colo-rectal end to end anastomosis, using a 31 mm CEEA-Stapler. The resected sigmoid colon contained the lost partial denture, which showed impaction and perforation into the sigmoid mesocolon (Fig. 4). Following surgery, the patient was transferred to the surgical ICU for 24 h observation and discharged home after one week.
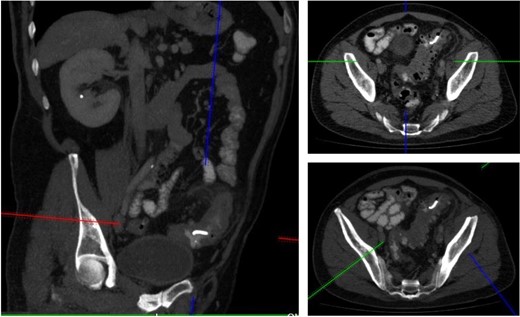
CT imaging identified a small curvilinear metallic foreign body within the sigmoid colon.

PFA showed the persistent presence of a metallic foreign body over the sigmoid colon.
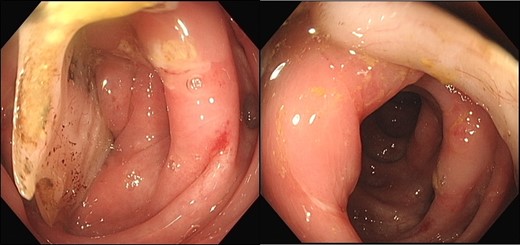
Colonoscopy identified a non-retrievable foreign body impacting the lumen of the sigmoid colon.

22 cm of resected sigmoid colon contained the lost partial denture showing impaction and perforation into the sigmoid mesocolon.
DISCUSSION
Foreign body ingestion (FBI) is a common clinical entity encountered in A&E. Most ingested foreign bodies pass the digestive tract without complications, whereas 10–20% of the cases require an interventional procedure such as endoscopy [1]. Apart from fish- and chicken bones, batteries, tooth picks and coins, dentures are the most common ingested foreign bodies [1, 2]. If ingested, dentures can cause serious complications such as impaction or bowel perforation [3–6]. A delay in the diagnosis can result in significant morbidity with fatal outcome even in younger patients [3]. One reason is that foreign body ingestions often go unnoticed. A recent review by Samast et al. on 21 cases of GI-tract perforation revealed that 81% did not recall a foreign body ingestion at the time of admission [1]. The strongest risk factor for failure of recollection seems to be the wear of dentures as it reduces the sensation of the palate. This is supported by Rodríguez‐Hermosa et al. who reviewed 33 cases of intestinal perforation due to involuntary foreign body ingestion. In 72% of the cases, the patients did wear a denture [2]. Other risk factors are mechanical falls, hurried eating, mental diseases, alcohol- and drug abuse. Furthermore, dentures are made from polymethylmethacrylate (PMMA), a denture base material, which is radiolucent and thus extremely difficult to visualize on conventional imaging [5, 7]. To date not all dentures contain radiopaque material. Our case report refers to a 52-year old male patient that presented to the A&E with typical features of a new flare of diverticulitis, as with previous admissions. However, with the repeat CT scan the small metallic compound of the patient’s partial denture was identified and appropriate measures were taken. In view of the fact that foreign body ingestions often go unnoticed, clinicians should maintain a high level of suspicion in patients with GI-tract perforation and above-mentioned risk factors. We conclude that all dentures should contain a radiopaque marker in order to avoid failure in radiological detection and prevent misdiagnose and inappropriate treatment.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.
CONSENT
Written informed consent was obtained from the patient for publication of this case report, including accompanying images.



