-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua N Hammerschlag, Clemente Chia, Chaminda Saranasuriya, Prostate cancer recurrence presenting as an isolated small bowel tumour, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz065, https://doi.org/10.1093/jscr/rjz065
Close - Share Icon Share
Abstract
Prostate cancer is the most commonly diagnosed cancer in males and third most common cause of cancer deaths in Australia. With improved survival rates and increasing reports of metastatic disease, we can expect to see more interesting and unusual presentations of recurrent disease. We present the case of a 66-year-old male with a prostate cancer recurrence to small bowel after curative treatment. We present this case to raise clinical suspicion in the medical fraternity regarding cancer recurrence; Even in the absence of biochemical markers or typical clinical signs and symptoms.
INTRODUCTION
We present the case of a 66-year-old male with a solitary small bowel tumour that was discovered to be prostate cancer recurrence despite prior curative treatment. Despite improved survival rates in prostate cancer and increasing reports of metastatic disease, this unique presentation has not previously been reported in scientific literature.
CASE REPORT
A 66-year-old male with hypertension and type 2 diabetes mellitus was referred to our institution in June 2015 for investigation of haematuria, urinary retention and lower abdominal pain with associated PR bleeding. CT scan revealed a large prostatic abscess, invading into rectum. A TURP was performed to de-roof the abscess. Histopathology demonstrated a poorly differentiated prostatic adenocarcinoma with extensive necrosis. Colonoscopy was arranged to investigate the extent of invasion into rectum and the patient was presented at a multidisciplinary team meeting. The consensus decision was to perform a total pelvic exenteration, abdominoperineal resection with end sigmoid colostomy and ileal conduit formation. Histopathology confirmed a Gleason 5 + 5, T4N0M1 prostatic adenocarcinoma with six liver metastases on further imaging. The patient was started on hormonal therapy with Firmagon and Zoladex and completed six cycles of chemotherapy by 2016.
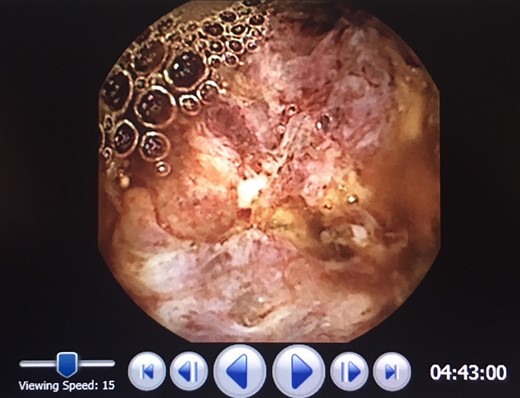
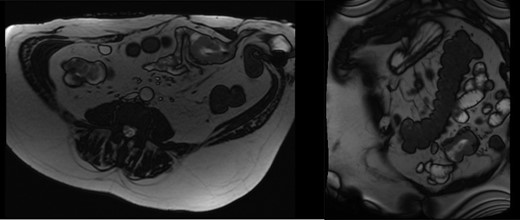
In 2017, repeat imaging showed resolution of all liver metastases, and the patient’s PSA was <0.1. While he had responded excellently to treatment, the patient had developed parastomal hernias around both the colostomy and ileal conduit. Between 2015 and 2017, the patient presented to hospital twice with features suggestive of small bowel obstruction. At the time, this was believed to be related to the hernias and therefore, the patient was planned for surgical repair of these hernias. During pre-operative workup, investigations revealed the patient to be anaemic with a haemoglobin of 80 and a ferritin of 11. Gastroscopy and colonoscopy revealed no abnormality; however, a pill cam demonstrated a single large lesion in the jejunum (Fig. 1). An MRI enterography was arranged to further characterize the lesion (Fig. 2). Given the excellent response to treatment, resolution of all liver metastasis and undetectable PSA levels a prostate cancer metastasis was not suspected. As the nature of this lesion was uncertain, a decision was made to perform a diagnostic laparotomy at time of hernia repair with small bowel resection if indicated.

The patient underwent a laparotomy, and a mass was discovered in the mid small bowel (Fig. 3). A small bowel resection was performed, followed by repair of both parastomal hernias with biological mesh. Histopathology showed poorly differentiated adenocarcinoma with positive Prostate-specific membrane antigen (PSMA) staining consistent with prostat cancer metastasis. The patient was referred to oncology for further treatment. On review two months later, the patient had recovered well from surgery with no signs of hernia recurrence.
DISCUSSION
Prostate cancer is the most commonly diagnosed cancer in males and third most common cause of cancer deaths in Australia. Recent advances in management have improved 5-year survival rates from 58% in 1984 to 95% in 2009 [1] and the incidence of metastatic prostate cancer has significantly increased over the last 10 years [3]. As such it is likely that rarer sites of metastases will be discovered with increasing frequency.
An autopsy study of 1589 cases of prostate cancer revealed the most common sites of metastases include bone (90%), lung (46%), liver (25%), pleura (21%) and adrenals (13%) [2, 4] Metastases to the gastrointestinal tract are rare, and are usually a result of localized invasion of the rectum. A second autopsy study found 76% of patients who died of metastatic prostate cancer had extensive intra-abdominal disease, however isolated cases of metastases to small bowel are extremely rare [2, 5], with only three reported cases in the literature [6–8]. All three cases differ significantly to the case presented as the tumour was isolated, without metastatic disease and the patient was seemingly asymptomatic, given the obstructive symptoms were most likely to be related to the patient’s hernias.
At first diagnosis, the patient was found to have liver metastasis. However, following treatment, there was complete resolution of these lesions and his PSA level was undetectable. PSA levels have been found to play an important role in the screening for disease recurrence in prostate cancer, and a detectable serum PSA may be the only evidence of cancer recurrence [9]. Despite PSA having a sensitivity of 72.1% in the detection of prostate cancer [10], reports of disease recurrence in patients with negative PSA are rare [9]. This further adds to the intrigue of this unique case.
Prostate cancer poses a significant disease burden on society and metastatic disease poses an ongoing challenge for future cancer management. This report outlines an extremely unusual case of a solitary metastatic deposit in an unlikely location. Moreover, it was incidentally discovered in a patient who was seemingly cured of his disease. It is hoped that this case will increase the index of suspicion for future patients presenting with gastrointestinal symptoms or masses and a history of prostate cancer.
DISCLOSURE STATEMENT
The authors have no conflict of interest to disclose. No financial support was obtained
CONFLICT OF INTEREST STATEMENT
None declared.



