-
PDF
- Split View
-
Views
-
Cite
Cite
Reena Thakrar, Sherif Monib, Emre Pakdemirli, Simon Thomson, Calcified gallbladder cancer: is it preventable?, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz069, https://doi.org/10.1093/jscr/rjz069
Close - Share Icon Share
Abstract
A case of a newly diagnosed calcified gallbladder cancer is presented, who had pre-existing porcelain gallbladder. Due to the advanced stage of the disease at presentation, the patient had a poor outcome. The investigation and management of gallbladder carcinoma is discussed as well as the relationship with porcelain gallbladder. We conclude that there is only a weak association between porcelain gallbladder and gallbladder cancer, but because gallbladder cancer typically presents late, a stratified approach to offering cholecystectomy to asymptomatic porcelain gallbladder is reasonable.
INTRODUCTION
Porcelain gallbladder (PGB), or calcified gallbladder, is a rare finding in 0.05–0.08% of cholecystectomy specimens [1]. PGB may be associated with gallbladder cancer (GBC) in over 60% of cases [2] and many asymptomatic patients with confirmed PGB will have a laparoscopic cholecystectomy to treat current or prevent future malignancy [3]. However, modern techniques for imaging have led to earlier and more frequent detection of PGB [4], resulting in a much reduced rate of GBC among patients with PGB and leading to the suggestion that cholecystectomy is not indicated for asymptomatic PGB [5]. We present a case of late symptomatic presentation of calcified GBC in a patient who had the incidental finding of a partially calcified gallbladder on ultrasound scan 8 years previously. We reassess current evidence for the management of porcelain gallbladder.
CASE REPORT
A 65year-old female presented with a 3-week history of intermittent epigastric pain, nausea, vomiting and weight loss and a past medical history included poor mobility, type II diabetes and hypercholesterolaemia. 8 years previously she had been admitted with E. coli sepsis and diarrhoea and an ultrasound scan (US) at the time had incidentally shown a partially calcified gallbladder with no features of inflammation and with benign fatty changes in the liver. With her ongoing comorbidities, no further intervention was recommended at the time.
On the current admission, general examination was unremarkable and vital signs were normal. Abdominal examination revealed no organomegaly or palpable mass. Blood tests showed deranged liver function tests (ALT 45 U/l, ALP 775 U/l, total bilirubin 20umol/l, albumin 27 g/l, GGT 553 U/l), hypercalcaemia (adjusted calcium 2.73 mmol/l) and leukocytosis (WCC 10.8 × 109/l). US showed the gallbladder had poor delineation of the posterior wall and appeared large, solid and heterogenous with posterior dense shadowing and with calcific components. Where visualized, the CBD was of normal calibre and no intrahepatic duct dilatation was seen. There was a large, ill-defined heterogenous mass within the liver (Fig. 1). Subsequent computerized tomography (CT) showed a10cm solid porcelain gallbladder invading liver segments 4 and 5 (Fig. 2), with evidence of enlarged coeliac, peri-pancreatic and para-aortic lymph nodes as well as pulmonary metastatic deposits (T4 N1 M1).
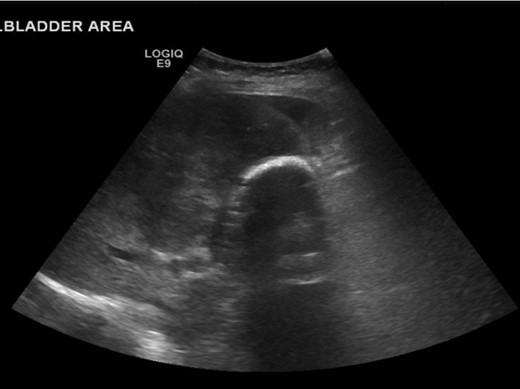
US showing porcelain gallbladder with a posterior acoustic shadow.
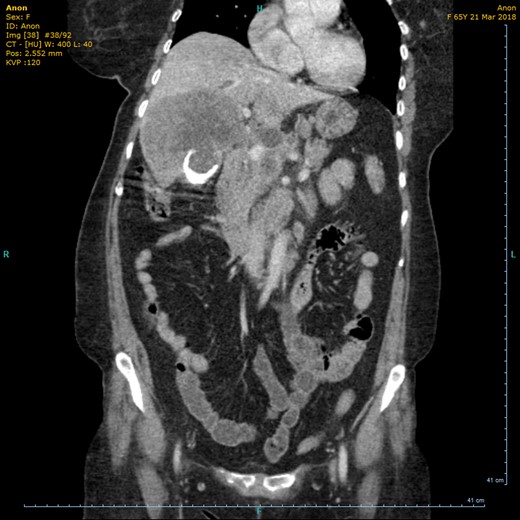
CT (coronal view) showing circumferential calcification in the thickened wall of the gallbladder.
To fully assess for management options, the regional hepatobiliary multidisciplinary meeting recommended magnetic resonance cholangiopancreatography (MRCP) and a liver biopsy. MRCP showed extensive gallbladder tumour involving adjacent parenchyma (Fig. 3), dilated intrahepatic bile ducts with a trace peri-hepatic fluid, scattered satellite liver metastases, bilateral lung metastases and extensive peri-portal, portocaval and upper retroperitoneal lymph nodes. US-guided liver biopsy confirmed metastatic adenocarcinoma consistent with a pancreatico-biliary system, gall bladder or upper gastrointestinal tract primary site. These results negated any active management of the condition and the patient was therefore discharged on a palliative care pathway. She was admitted 2 weeks later with diffuse abdominal pain, ascites, which was subsequently drained, but she clinically deteriorated and passed away 4 weeks later.

MRCP shows gallbladder fundus with a T2 weighted hypo intense rim.
DISCUSSION
The term PGB specifically refers to the ‘blue’ discoloration and brittle consistency of the gallbladder wall, but in literature is more often used to describe all types of gallbladder calcification [4]. It is more common in women, between 50 and 70 years, associated with gallstones in 90% of cases and found in <1% of cholecystectomy specimens [1, 6].
There is no definitive consensus on the incidence rate of GBC from PGB but is estimated to range from 12.5% to 61% [7] other studies suggested a lower incidence of 0–5% however in any case, it still represents a statistically significant risk factor of developing GBC [3].
Types of gallbladder calcification include selective mucosal calcification and diffuse intramural calcification, the latter having a greater affiliation with PGB [3]. Its exact aetiology is poorly understood, however is thought to be as a result of chronic inflammation of the gallbladder wall [8]. Errors in calcium metabolism and abnormal calcification are implicated in the formation of PGB such as obstruction of cystic ducts leading to calcium deposits in the mucosa, subsequent degeneration and regeneration process within gallbladder epithelium or offensive chemicals in stagnant bile salts which may lead to mucosal dysplasia and later progress to cancer. Carcinomas associated with PGB are diffusely infiltrating adenocarcinomas [8, 9].
PGB patients are usually asymptomatic, diagnosed as incidental findings on imaging. The radiological appearance of a calcified gallbladder varies based on the extent and location of calcification. US is useful for identifying abdominal pathologies, however, the diagnosis can be challenging because there are several common differentials such as large opaque gallstones, acute cholecystitis or calcified liver/renal cysts which may closely mimic PGB. In addition, the findings on US can be non-specific [10].
Painless jaundice, unexplained weight loss, abdominal pain/bloating and/or a palpable mass are possible predictors of gallbladder cancer. Unfortunately, as in our presented case, the presence of these is also indicative of advanced malignancy, where curative surgery is not feasible and therefore they have limited clinical value [3]. In cases where a diagnosis of GBC is confirmed, an accurate assessment of TNM stage is crucial to plan further treatment and/or surgery. Other complimentary imaging modalities such as MRI and MRCP can provide further information on this. Diagnostic laparoscopy should be used in select patients to avoid unnecessary laparotomy [11].
Recent recommendations for patients with incidentally diagnosed GBC at laparoscopic cholecystectomy are to undergo re-resection for T1b, T2 or T3 disease, as the presence of residual disease is associated with decreased survival. Major hepatectomy and common bile duct excision should only be performed in select cases. Current standard of care for adjuvant therapy includes 6 months of oral capecitabine. Gemcitabine-cisplatin is the standard of care therapy for advanced-stage disease [11].
Houry S et al. highlighted that gallbladder carcinomas are not as radioresistant as was formerly thought. Local control of the tumour and reduction of tumour size was reported in several publications. Their data showed a slight improvement of survival after adjuvant or palliative radiotherapy, especially in the advanced stage of gallbladder carcinomas. They recommend an intraoperative 15 Gy boost (brachytherapy) and an additional 45–50 Gy post-operatively [12]. More recently, Xiao-Nan Sun et al have demonstrated better sparing of surrounding tissues whilst maintaining effective target coverage using intensity-modulated radiotherapy [13].
Management of gallbladder wall calcifications has been controversial with no clear guidelines for many decades. Although the traditionally perceived strong association with gallbladder cancer, sometimes quoted at over 60%, mandated prophylactic cholecystectomy, this was largely based on papers from before 1962 and newer evidence suggests a much lesser association which may indicate a more selective or an observational approach [3, 7, 14, 15]. A review from 2013 found GBC in only 6% (0–33%) of PGB compared to 1% (0–4%) in a matched cohort of patients without gallbladder wall calcification [3]. It is also noteworthy that the vast majority of GBC do not exhibit calcification, a series of 88 GBC not finding any such cases [16]. We do not know of any prospective series of asymptomatic PGB undergoing observational follow-up and the exact relationship with GBC is therefore unclear, as is the significance of degree of calcification (partial, as in our case, or complete).
On this basis, there is support for not having proceeded to cholecystectomy in our patient, who had significant comorbidities when she was first diagnosed with incidental PGB, it being more probably that her GBC was not a direct consequence of the pre-existing PGB. Indeed, the strongest risk factor for GBC is gallstones, which were not present. However, as PGB still represents a low but significant risk, we would recommend that cases be discussed in an appropriate multidisciplinary meeting and, with the current drive towards greater patient involvement in decisions over their care, to discuss the possible risks and future management with the patient. A stratified approach of recommending cholecystectomy to younger and fitter patients would be reasonable.
CONCLUSION
Porcelain gallbladder is a rare condition that has traditionally been regarded as premalignant, although the exact relationship remains unclear and current evidence shows its association with gallbladder cancer to be weak. In some centres, the trend is therefore away from routine cholecystectomy for porcelain gallbladder, despite the majority of gallbladder adenocarcinomas being picked up at a late stage where curative treatment is not possible. It would be appropriate to discuss individual cases of asymptomatic porcelain gallbladder in an appropriate multidisciplinary meeting, the risks explained to the patient and to adopt a stratified approach to recommending cholecystectomy.
CONFLICT OF INTEREST STATEMENT
None declared.



