-
PDF
- Split View
-
Views
-
Cite
Cite
Yuhei Waki, Ryo Ashida, Teiichi Sugiura, Yukiyasu Okamura, Takaaki Ito, Yusuke Yamamoto, Katsuhisa Ohgi, Katsuhiko Uesaka, Pancreatoduodenectomy with an anomalous common hepatic artery and the left gastric artery arising from a common trunk, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz066, https://doi.org/10.1093/jscr/rjz066
Close - Share Icon Share
Abstract
A 67-year-old woman with epigastric pain was diagnosed with resectable pancreatic head cancer and underwent pancreatoduodenectomy. Preoperative computed tomography showed that the common hepatic artery formed a common trunk with the left gastric artery running to the liver through the lesser omentum, and no other arterial supply to the liver was identified. Pancreatoduodenectomy was performed uneventfully without injury to any hepatic arteries. The postoperative clinical course was largely uneventful, and the patient was discharged on postoperative day 19. An anatomical variation of the common hepatic artery arising from a common trunk with the left gastric artery and coursing within the lesser omentum is rare. Notably, this is the first case report of pancreatoduodenectomy with this anatomical variation. Thorough understanding of hepatic arterial anatomical variations is necessary to prevent complications caused by inadvertent vascular injury and hepatic ischemia.
INTRODUCTION
Pancreatoduodenectomy is the standard treatment for resectable periampullary cancer. Despite improvements in surgical technics and devices, the morbidity and mortality rate after pancreatoduodenectomy remain relatively high [1, 2]. During pancreatoduodenectomy, hepatic arterial injury and/or ischemia can lead to potentially lethal complications. Thus, a thorough preoperative understanding of arterial anatomy is necessary [2].
We recently encountered a patient who underwent pancreatoduodenectomy with a rare hepatic arterial variation. The common hepatic artery (CHA) arose from a common trunk with the left gastric artery (LGA), with a course through the lesser omentum as the only arterial supply to the liver [3]. Fewer than 10 cases of this variant have been described worldwide [4]. To our knowledge, this is the first report of a patient who underwent pancreatoduodenectomy with this anatomical variant.
CASE REPORT
A 67-year-old woman with a 1-month history of epigastric pain was referred to our hospital with suspected pancreatic head cancer. Endoscopic ultrasonography and fine-needle biopsy of the tumor revealed adenocarcinoma of the pancreatic head. Computed tomography (CT) showed a 17 × 12 mm hypovascular tumor without arterial or portal venous invasion in the pancreatic head, and the CHA formed a common trunk with the LGA, coursing within the lesser omentum (Fig. 1). In addition, preoperative three-dimensional CT angiography revealed that the celiac artery branched into the splenic artery and the common trunk, and the usual CHA was absent in the supra-pancreatic area. The CHA formed a common trunk with the LGA and arched in a cranial direction within the lesser omentum immediately adjacent to the liver. No other arterial supply to the liver was identified (Fig. 2). With the preoperative diagnosis of resectable pancreatic head cancer and clinical staging of T2N0M0 (UICC 8th edition), pancreatoduodenectomy was planned.
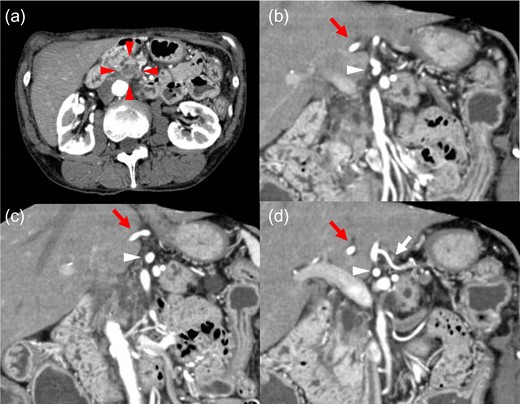
Axial and reconstructed coronal contrast-enhanced CT. (a) Axial contrast CT image showing a 17 × 12 mm hypovascular tumor in the pancreatic head (red arrowhead). No enlarged lymph nodes or distant metastases were detected. (b–d) Coronal contrast CT image showing the CHA (red arrow) forming a common trunk (white arrowhead) with the LGA (white arrow) and coursing within the lesser omentum. CHA: common hepatic artery. LGA: left gastric artery.
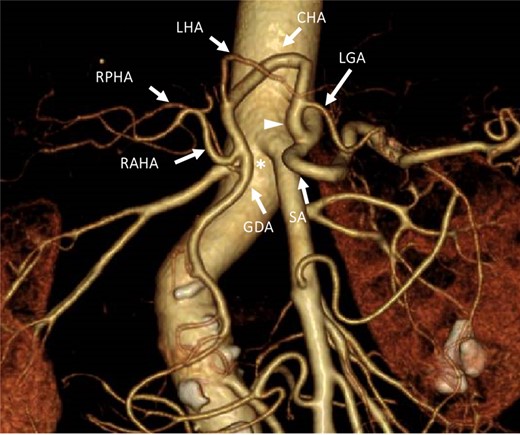
Three-dimensional computed tomography angiographic image from an anteroposterior view. The celiac artery branched into the SA. A common trunk (white arrowhead) branched into the LGA and the common hepatic artery, which arched toward the cranial side. No arterial bridge existed between the celiac trunk and the GDA (asterisk). LGA: left gastric artery. CHA: common hepatic artery. SA: splenic artery. LHA: left hepatic artery. RAHA: right anterior hepatic artery. RPHA: right posterior hepatic artery. GDA: gastroduodenal artery.
Intraoperatively, the CHA was identified in the lesser omentum, forming a common trunk with the LGA as shown on preoperative CT. As the first step of lymph node dissection in the hepatoduodenal ligament, the gastroduodenal artery was identified and taped carefully in the supra-pancreatic area. Second, the gastroduodenal artery was skeletonized cranially, with taping of the right anterior hepatic artery, the right posterior hepatic artery, the left hepatic artery, and the CHA in turn. Third, after the anterior surface of the portal vein was exposed in the supra-pancreatic area in the absence of the CHA, the tissue and lymph nodes along the portal vein were completely skeletonized toward the hepatic hilum. Before dividing the vessel, we clamped the gastroduodenal artery and confirmed blood flow in the intrahepatic arteries using ultrasonography. During skeletonization, we were careful to avoid vascular injury to both the portal vein and common trunk coursing within the lesser omentum. Finally, the common bile duct was divided at the level of the junction of the cystic duct, and pericholedochal tissue and the lymph nodes of the bile duct were dissected. No arterial vestiges of the usual CHA were found in the supra-pancreatic area (Fig. 3). The pancreatoduodenectomy procedure including lymph node dissection was completed as usual, without injury to any hepatic arteries (Fig. 4).
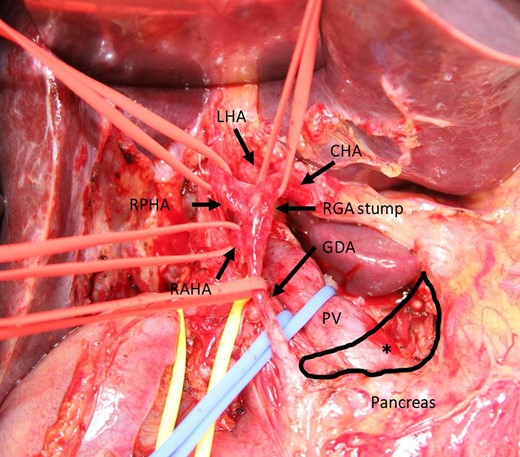
Intraoperative photograph during dissection of the hepatoduodenal ligament. The CHA arose from the lesser omentum. The RPHA, RAHA, and GDA were taped just distal to branching of the trunk. The PV was taped behind the GDA. No arterial vestige of the usual CHA was found in the supra-pancreatic area (asterisk). CHA: common hepatic artery. LHA: left hepatic artery. RAHA: right anterior hepatic artery. PHA: right posterior hepatic artery. GDA: gastroduodenal artery. PV: portal vein. RGA: right gastric artery.
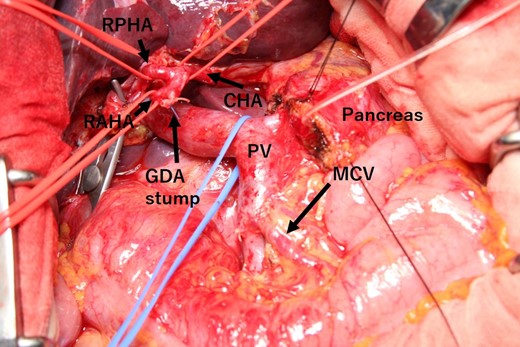
Intraoperative photograph after removal of the specimen. The CHA arose from the lesser omentum. The CHA, RPHA, and RAHA were taped, and all hepatic arteries were preserved. CHA: common hepatic artery. MCV: middle colic vein. RAHA: right anterior hepatic artery. RPHA: right posterior hepatic artery. GDA: gastroduodenal artery. PV: portal vein.
The postoperative course was largely uneventful except for mild delayed gastric emptying. The patient was discharged on postoperative day 19. The microscopic findings revealed invasive ductal carcinoma of the pancreas with lymph node metastasis. The patient received adjuvant chemotherapy and developed recurrence of lymph nodes.
DISCUSSION
In 50–75% of cases, the CHA arises from the celiac artery [5]. Although the CHA occasionally arises from the superior mesenteric artery or abdominal aorta, the incidence of these variations is reportedly 1–4% and 0.2–0.7%, respectively [4]. An anatomical variation of the CHA arising from a common trunk with the LGA and coursing within the lesser omentum is rarely seen [6]. Nine cases with this variation have been reported worldwide, with an incidence of 0.4–0.5% [6, 7]. To our knowledge, this is the first case report of pancreatoduodenectomy with this anatomical variation.
Different patterns of regression of embryologic precursor arteries may explain the variations. The aforementioned rare anatomical variation (as the only blood supply to the liver) originates from abnormal regression of the middle embryonic artery and persistence of the left embryonic artery [7].
A CHA arising from a common trunk with the LGA within the lesser omentum is an important variation of the hepatic artery from a surgical point of view. First, accidental ligation or injury of this artery, especially when dividing the lesser omentum, might lead to clinically significant hepatic ischemia requiring reconstruction of the hepatic artery, as this would then become the only arterial supply to the liver after pancreatoduodenectomy [8]. Second, during dissection in the supra-pancreatic area in the absence of the CHA, scrupulous attention is required to avoid injury and hemorrhage of the portal vein as well as to perform appropriate lymph node dissection according to oncological treatment criteria. In addition, confirming all anatomical variations of the hepatic arteries using taping and test clamping of arteries in the hepatic portal region may be necessary to avoid intraoperative complications and perform appropriate lymph node dissection.
Recently, multidetector row CT using volume-rendered images has improved the delineation of pancreatic lesions and vascular structures. Previous studies have focused on not only arterial but also portal-venous or venous imaging [9]. Therefore, routine preoperative CT angiography could aid in the identification of hepatic vascular anatomical variations, thereby preparing surgeons to better deal with these vascular anomalies intraoperatively and to ensure a safe surgical procedure [10].
In conclusion, this hepatic arterial anatomic variation should be carefully managed to prevent inadvertent vascular injury and hepatic ischemia, even if it is not identified on preoperative CT.
ACKNOWLEDGMENTS
The authors declare that they have no financial supports.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.



