-
PDF
- Split View
-
Views
-
Cite
Cite
S Gussago, P Spina, A Guerra, Benign Multicystic Peritoneal Mesothelioma (BMPM) as a rare cause of abdominal pain in a young male: case report and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz057, https://doi.org/10.1093/jscr/rjz057
Close - Share Icon Share
Abstract
Benign Multicystic Peritoneal Mesothelioma (BMPM) is a rare benign cystic neoplasm that arise from the peritoneum, typically found in young females (83%), with a high incidence of local recurrence after resection (almost 50% of cases). Fewer than 200 cases have been reported worldwide in 2017. Due to its rarity and the lack of a classical clinical presentation, the diagnosis pre-operatively is challenging; moreover a great part of the literature is composed of case reports and small group studies. Nowadays, guidelines are still not available, and treatment is en bloc resection of the lesion. Some authors suggest the use of Hyperthermic Intraperitoneal Chemotherapy (HIPEC) associated with the surgical approach, even if comparative data on recurrence and complications are lacking. We report a case of BMPM diagnosed in a 40-year-old male who underwent an exploratory laparoscopy and complete excision of the neoformation. Pathology confirmed the presence of a BMPM.
INTRODUCTION
Benign Multicystic Peritoneal Mesothelioma (BMPM) is an exceedingly rare benign cystic intra-abdominal neoplasy that arise from the peritoneum [1], typically found in females of child-bearing age [2], with a high incidence of local recurrence [3] after surgical resection, even after a long silent follow-up [4]. First described in 1979 by Mennemeyer and Smith, fewer than 200 cases have been reported worldwide in 2017 [5]. Although classically described as a benign lesion, with low risk of show malignant transformation and only after repeated postoperative recurrences, a case report described malignancy since its first manifestation. Pathogenesis of this neoplasm is still uncertain; association with previous abdominal surgery, endometriosis or pelvic inflammatory disease are described [6]. Symptoms are non-specific, such as abdominal or pelvic pain and mass, but this entity may be found incidentally at laparotomy or within a hernia sac, grossly composed of multiple cysts measuring up to 15 cm or more in diameter, microscopically lined by mesothelial cells. Due to its rarity, preoperative diagnosis is still a challenging clinical problem [6]. No evidence-based guidelines for treatment are actually available, although a surgical resection is recommended: some authors suggest a combination of cytoreductive surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) [7], and new strategies based upon immunohistochemistry knowledge of the neoplasm may lead to others pharmaceutical strategies [8]. Benign Multicystic Peritoneal Mesothelioma (BMPM) is a rare benign cystic neoplasm that arise from the peritoneum, typically found in young females (83%), with a high incidence of local recurrence after resection (almost 50% of cases). Fewer than 200 cases have been reported worldwide in 2017. Due to its rarity and the lack of a classical clinical presentation the diagnosis pre-operatively is challenging, moreover a great part of the literature is composed of case reports and small group studies. Nowadays, guidelines are still not available, and treatment is en bloc resection of the lesion. Some authors suggest the use of HIPEC associated with the surgical approach, even if comparative data on recurrence and complications are lacking. We report a case of BMPM diagnosed in a 40-year-old male who underwent an exploratory laparoscopy and complete excision of the neoformation. Pathology confirmed the presence of a BMPM.
CASE REPORT
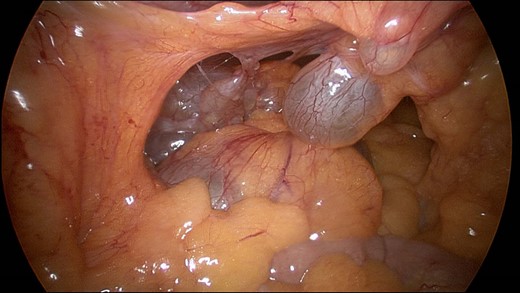
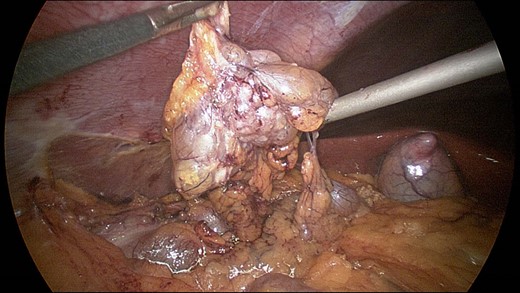
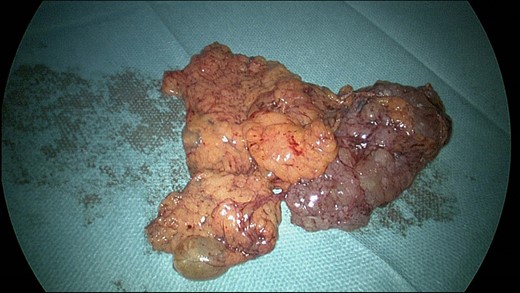
A 40-year-old Caucasian male, a past medical history of smoking, complaining from 5 years of occasional abdominal discomfort started having an acute, stinging pain in the right upper abdomen. A blood sample was taken that showed a smoldering increase of the transaminases and C-reactive protein of 22 mg/L. He was investigated in the outpatient setting with an abdominal ultrasonography that revealed a polycystic lesion of 9 cm of diameter in the right flank. He was than referred to our Hospital, where the physical examination was completely silent. A contrast enhanced CT scan of the abdomen revealed a polylobate hypodense formation, with multiple thin internal septa which are enriched after contrast (dimension 83 × 43 × 61 mm) (Figs 1 and 2). Radiologist posed differential diagnosis among peritoneal lymphangiomatosis, enteric duplication cyst and—even if less likely in a male without history of past abdominal surgery—benign multicystic peritoneal mesothelioma. After multidisciplinary discussion we proceeded to an exploratory laparoscopy that confirmed the presence of multiple cystic lesions of the peritoneum, some interesting the omentum, with a weak adherence with the ascending colon (Figs 3 and 4). We performed a complete excision of the neoformation, with free margin on omental fat. A small lesion of the colonic serosa was treated with a prophylactic continuous suture with Vycril 2-0. The postoperative course was uneventful ant the patient was discharged after 2 days without complications.

Computed tomography image results: (1) contrast enhanced sagittal reconstruction showing the right flank neoplasm.
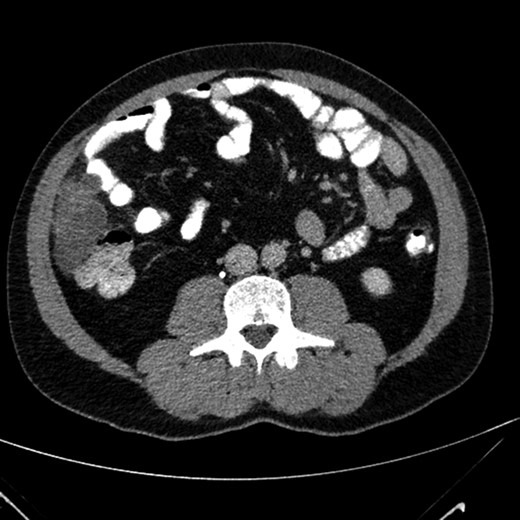
Contrast enhanced axial image that show the presence of a polylobate hypodense formation, with multiple thin internal septa.
On gross examination a soft, yellowish tissue specimen was seen, measuring about 13 × 9 × 4 cm, composed of multiple cysts, up to 1 cm in diameter, containing a clear fluid. It was fixed in 10% formalin, embedded in paraffin, and the sections were evaluated by hematoxylin and eosin stain. Histologically, it consisted of cysts lined by a single layer of flattened to cuboidal mesothelial cells without atypia. Immunohistochemistry using an automated stainer (Ventana, Tucson, AZ) was performed and all tumor cells showed immunoreactivity for WT1 and Calretinin. Based on these findings, the final histological diagnosis was multicystic benign mesothelioma.
After discussion with Referral Center was suggested an annual follow-up with MRI, and in case of relapse an approach with cytoreductive surgery and subsequent HIPEC.
DISCUSSION
Even if other case reports described this condition, is particularly uncommon to find BMPM in young male patients without a past medical history of intra-abdominal surgery.
Clinical presentation usually includes chronic abdominal discomfort and mass-related symptoms like abdominal distension, tenderness or dyspareunia. Physical examination may notice an abdominal mass. At the time of diagnosis, the mean diameter of BMPM is 13 cm [3]. Ultrasound of the abdomen usually shows anechoic to mildly echogenic, multiseptated cystic structures in the pelvis composed of some lobulations and cysts [9].
On CT scan, BMPM usually appears as low-density, multi-loculated, multicystic, thin-walled lesion. On MRI, BMPM appears hypointense on T1-weighted images and with hyper to intermediate intensity on T2-weighted sequences, with mild contrast enhancement of the wall [9].
On radiological imaging abdominal lymphangioma is the most important differential diagnosis, but this neoplasm is more typical of pediatric population. The differential diagnosis must include cystic adenomatoid tumor and malignant mesothelioma (Figs 5–8).
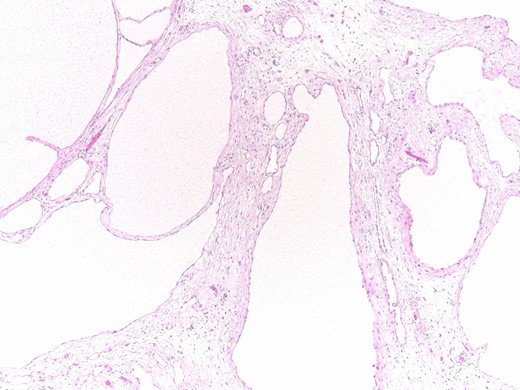
Histopathology results: cysts lined by flattened/cuboidal mesothelial cells.
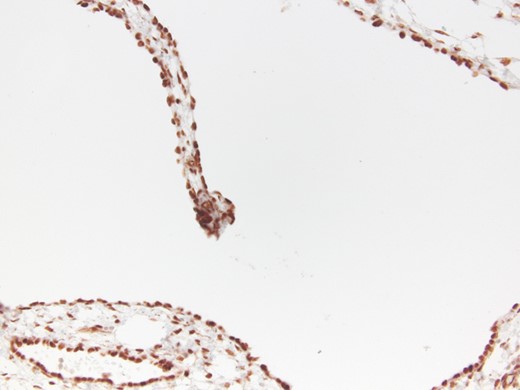
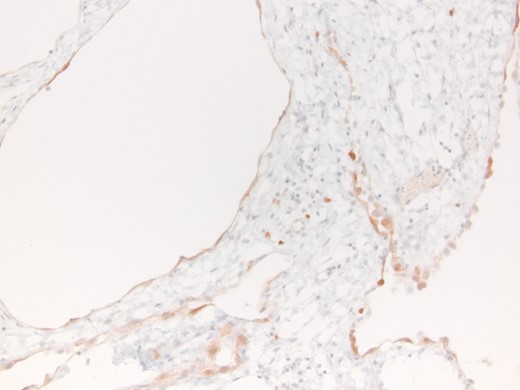
Microscopically, the cysts of BMPM are lined by cuboidal or flattened mesothelial cells. In the latter case, BMPM could simulate the appearance of a cystic lymphangioma, but the former exhibits mesothelial markers, such as calretinin and WT1. Ross et al. [10] believe that BMPM is probably the result of a peritoneal reactive proliferation, forming multiple peritoneal inclusion cysts, and not a true neoplasm. The natural history of this disorder, with its great tendency to local recurrence and its tumor-like appearance, suggests its neoplastic pathogenesis, but both of the hypothesis can be argued.
Surgical resection en bloc of the BMPM is both diagnostic and therapeutic and usually performed with a laparoscopic approach, but it is affected by an high rate of recurrence. The extreme rarity of this pathology is the prominent limitation to an evidence-based approach. Nowadays, guidelines are still not available, even if some authors suggest the combination of cytoreductive surgery and HIPEC [7]. Chemotherapy and radiotherapy did not show effects in this neoplasm [1]. An interesting case report of 2017 described the use of Rapamycin after primary surgery since the high level of phosphorylation of p70S6 kinase, a downstream mTOR target, found in BMPM [8]. No time lapse of follow up is known, with recurrence of this pathology reported as far as 36 years after surgery.
A better knowledge and consequent probably better therapeutic approach for BMPM could be gained by a centralization of cases in National Reference Centers, in order to increase the volume of patients and allow the beginning of targeted studies. Even if BMPMs are affected by an extremely low rate of mortality (one case report) [2], the high risk of recurrence of this neoplasm brings an intrinsic moderate–high morbidity, with a considerable need for prolonged follow-up, particularly in young women whom infertility related radiation risk must be considered.
CONFLICT OF INTEREST STATEMENT
None declared.



