-
PDF
- Split View
-
Views
-
Cite
Cite
Salman Alsabah, Rawan Elabd, Jonathon D Vaz, Endoscopic versus laparoscopic management of an eroded mesh in vertical banded gastroplasty: video case series and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz060, https://doi.org/10.1093/jscr/rjz060
Close - Share Icon Share
Abstract
Vertical banded gastroplasty (VBG) was one of the most common bariatric surgeries worldwide in the beginning of the 21st century. However, recently we have increasingly encountered its long-term complications. We present two cases of VBG mesh erosion, alongside videos for their management. The first is of a 35-year-old female that presented 10 years after her VBG, while the second is of a 38-year-old female presenting 9-years post hers. Patient one presented with weight regain, regurgitation, epigastric pain, and dysphagia. CT imaging showed staple-line dehiscence and foreign body inside the stomach. Patient 2's presentation was of weight regain. Upon further workup, she was diagnosed with mesh erosion. In case 1, an endoscopic approach was taken using Soehendra lithotriptor device, while for case 2, a laparoscopic approach was undertaken. Endoscopic management of mesh erosion post-VBG is not only safe and feasible but also less invasive and time-consuming than the laparoscopic technique.
INTRODUCTION
Vertical Banded Gastroplasty (VBG) was one of the most common bariatric surgeries worldwide in the beginning of the 21st century [1]. This procedure works by stapling the anterior and posterior gastric walls at a distance from the gastroesophageal junction (GEJ), creating a vertical pouch that is bounded inferiorly by a polypropylene band, which limits the caloric intake through reducing the gastric reservoir capacity. Generally, VBG was found to be effective in reducing weight and eliminating obesity-related co-morbidities, with an overall resolution rate of co-morbidities of 54–80% [2]; however, in the recent years, we have been increasingly encountering its long-term complications. When it comes to prosthesis erosion associated with VBG, previous endoscopic and laparoscopic management have been reported but a comparison between the two approaches remains lacking.
CASES PRESENTATION AND MANAGEMENT
We, in the video, compare and contrast the management of two cases of mesh erosion associated with VBG. The first case is a 35-year-old female with a BMI of 45.5 kg/m2 referred for the evaluation of an eroded VBG mesh. She had this procedure 10 years ago and successfully reached a BMI of 25.6 kg/m2 with an Excess Weight Loss (EWL) of 98.2% within two years. However, she presents now with weight regain, regurgitation, epigastric pain, and dysphagia. Barium study showed a disfigured GEJ while CT imaging showed staple-line dehiscence and foreign body inside the stomach with contrast stasis in the esophagus. Endoscopy later confirmed VBG mesh erosion as showed in Figs 1 and 2. On the other hand, the second case is a 38-year-old female with a BMI of 44 kg/m2 who had VBG done nine years ago. Her presentation was of weight regain. Upon further workup, she was diagnosed with mesh erosion and referred for laparoscopic management.
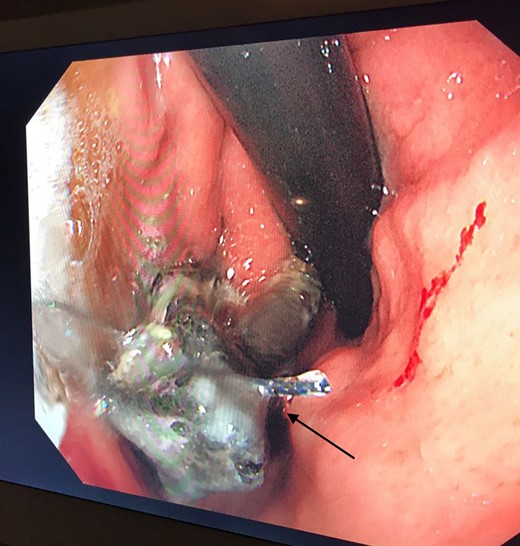
Retroflex endoscopic view of the mesh (black arrow) eroding into the stomach, 7 cm below the Gastroesophageal Junction (GEJ)-(Case 1).

Retroflex endoscopic view showing the mesh (black arrow) with an inflammatory polyp (blue arrow) mirroring it, likely due to inflammation-(Case 1).
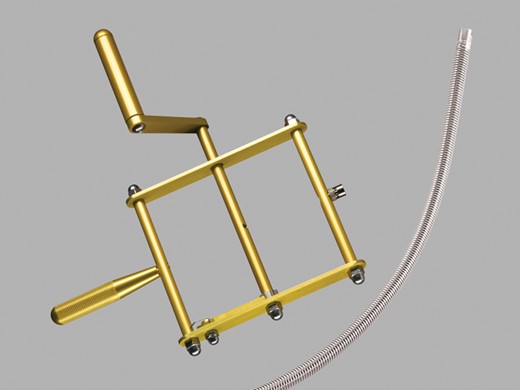
Concerning the management of our patients, in case 1, an endoscopic approach was taken. First, a guide wire was passed in between the eroded mesh and the stomach wall enabling us to circulate the mesh and divide it using Soehendra lithotriptor device (Fig. 3). Then the mesh, which is seen in Fig. 4, was completely removed endoscopically. In contrast, for case 2, a laparoscopic approach was undertaken. We started off with adhesion lysis to achieve a good anatomical view. Intraoperative endoscopy was used to understand the anatomy and locate the site of the eroded mesh followed by performing a gastrostomy to visualize and remove it, that is shown in Fig. 4. A comparison outlining the pros and cons of both techniques is presented in Table 1, and the video shows in detail the technique by which both approaches were carried out.
Comparison Between Laparoscopic versus Endoscopic Management of VBG mesh erosion.
| Factor . | Laparoscopy . | Endoscopy . |
|---|---|---|
| Time | 120 min | 20 min |
| Anatomy complexity | More | Less |
| Invasiveness | Invasive | Less invasive |
| Pain post-operation | More | Less |
| Mobility post-operation | Occurs later | Occurs earlier |
| Factor . | Laparoscopy . | Endoscopy . |
|---|---|---|
| Time | 120 min | 20 min |
| Anatomy complexity | More | Less |
| Invasiveness | Invasive | Less invasive |
| Pain post-operation | More | Less |
| Mobility post-operation | Occurs later | Occurs earlier |
Comparison Between Laparoscopic versus Endoscopic Management of VBG mesh erosion.
| Factor . | Laparoscopy . | Endoscopy . |
|---|---|---|
| Time | 120 min | 20 min |
| Anatomy complexity | More | Less |
| Invasiveness | Invasive | Less invasive |
| Pain post-operation | More | Less |
| Mobility post-operation | Occurs later | Occurs earlier |
| Factor . | Laparoscopy . | Endoscopy . |
|---|---|---|
| Time | 120 min | 20 min |
| Anatomy complexity | More | Less |
| Invasiveness | Invasive | Less invasive |
| Pain post-operation | More | Less |
| Mobility post-operation | Occurs later | Occurs earlier |

DISCUSSION
VBG has been in clinical use since 1979. The long-term results of this procedure are not as favorable as other bariatric surgeries, with it having a higher re-intervention and re-operation rate and lower patient quality of life [2]. Some VBG complications include gastroesophageal reflux [3], nausea and vomiting [3, 4], staple-line disruption [4], weight regain [4], and prosthesis erosion or migration [4]. Factors that increase the risk of erosion include infections, previous bariatric procedures, and surgical placement technique, which includes how tight the band was placed as narrower outlets were associated with necrosis and erosion [5]. Previous endoscopic removal has been successfully attempted in many patients who underwent different restrictive procedures with erosion. Specifically, when it comes to VBG with prosthesis erosion, Tai et al. has described the laparoscopic management of such a case [6]. Of more interest now is the endoscopic management of VBG failure and related complications. For example, Dietel and Bendago have described the endoscopic findings and revision of VBG complications, like dilatation of strictures or tightness [7], while similar management techniques were reported by others. When it comes to removal of an eroded VBG prosthesis, Karmali et al. [8] documented successful endoscopic scissor traction, while Nguyen et al. [9] reported endoscopic laser treatment for an obstructive VBG polypropylene mesh. Adam et al., in addition, reported endoscopic argon plasma coagulation for the management of Marlex mesh erosion after VBG [10]. We report the use of lithotripsy for endoscopic removal of an eroded mesh, and from our experience, the endoscopic approach of tackling prosthesis erosion associated with VBG is less invasive, faster, and less technically challenging than the laparoscopic technique (Fig. 5).
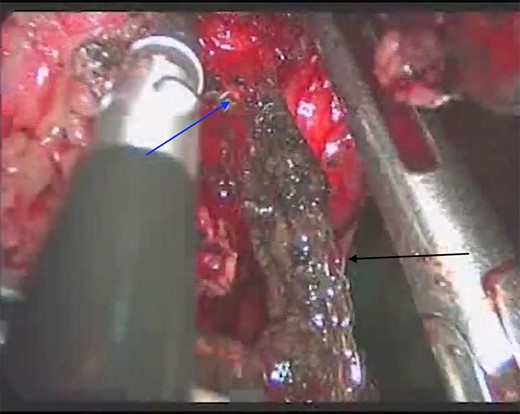
Laparoscopic view of the gastrostomy (blue arrow) and the mesh (black arrow) being removed from Case 2.
CONCLUSION
In conclusion, VBG procedure is associated with long-term complications and high re-operation rate. Endoscopic management of mesh erosion post-VBG is not only safe and feasible but also less invasive and time-consuming than the laparoscopic technique.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLAIMERS
None.
FUNDING OR SOURCES OF SUPPORT
None.
ETHICAL APPROVAL
An informed consent was obtained from the patients.



