-
PDF
- Split View
-
Views
-
Cite
Cite
Fabrizio Masciello, Aaron Fargion, Alessandro Alessi Innocenti, Elena Giacomelli, Luca Voltolini, Walter Dorigo, Carlo Pratesi, Open surgical conversion for Type II endoleak following hybrid treatment of a giant aneurysm of aberrant right subclavian artery, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz058, https://doi.org/10.1093/jscr/rjz058
Close - Share Icon Share
Abstract
Type II endoleak following hybrid treatment of aneurysms of aberrant subclavian arteries (AARSA) and requiring reintervention is rare. A retroesophageal AARSA with a 70 mm diameter was treated with left and right carotid to subclavian bypasses and thoracic endografting to exclude its ostium. The distal neck was embolized with a vascular plug. At 22 months postoperatively, an angio-computed tomography (CT) scan performed for worsening of dysphagia showed the presence of a Type II endoleak from bronchial arteries with significant sac enlargement. An open surgical repair with thoracotomy, aneurysmorraphy and ligature of the feeding vessels was successfully performed.
INTRODUCTION
Aberrant right subclavian artery, arising from the proximal descending thoracic aorta, is the most common anomaly of aortic arch, occurring in 0.4–1.9% of population [1]. This condition is usually asymptomatic. Surgical treatment is required if symptoms occur such as dysphagia, dysphonia, incoercible cough or when aneurysmal evolution (maximum diameter larger than 2 cm) is described [2, 3]. Even if rare, this condition can lead to potentially catastrophic complications such as rupture and thromboembolism [4]. Hybrid procedures, consisting in epiaortic vessel transposition or extra-anatomical bypasses followed by the coverage of the ostium with a TEVAR, are nowadays widely used [4]. The risk of developing late complications such as aneurismal reperfusion is described in the literature [5]; however, the need of open surgical conversion for treating sac enlargement is only anecdotally reported [4]. Herein, we describe the conversion to open repair of a giant aneurysm of an aberrant right subclavian artery (AARSA), previously treated with an hybrid approach, due to the development during follow-up of a Type II endoleak with aneurysmal sac enlargement. The patient gave the consent to use his personal data for scientific purpose.
CASE REPORT
A male patient, aged 73, with a history of hypertension and Pott Disease, was referred to our Unit for dysphagia and incoercible cough. The diagnostic angio-computed tomography (CT) scan showed a retroesophagel AARSA with a maximum diameter of 70 mm, determining the compression of both esophagus and trachea, with a dominant left vertebral artery (Fig. 1). Both aortic arch and thoracic aorta were not involved in the aneurysmal degeneration and no significant intra- and extracranic carotid stenoses were described. A hybrid surgical approach with was planned to exclude the AARSA and to preserve the inflow of both subclavian arteries. It consisted of a bilateral common carotid-to-subclavian artery bypass with a 7 mm expanded polytetrafluorethilene (ePTFE) prosthetic graft and the deployment of thoracic endoprosthesis (Cook Medical Inc, Bloomington, IL ZTA-P-40-117) distally to the left carotid ostium to exclude the aneurysm. The distal neck of AARSA was embolized with a 16 mm Amplatzer vascular plug. Complete technical success without evidence of endoleak was detected at the end of procedure. The embolization of the left subclavian artery at its origin was not performed because the stent-graft completely covered its ostium and it was well adherent to it. The postoperative medical therapy consisted of subcutaneous sodium enoxaparin for the first postoperative month and single antiplatelet treatment indefinitely. The patient was discharged on the ninth postoperative day and underwent angio-CT scan at 1 month (Fig. 2) and yearly thereafter. The 1-year angio-CT scan showed the development of a Type II endoleak from bronchial arteries without significant sac enlargement.


Twenty-two months after the procedure, the patient referred to our Unit due to the worsening of dysphagia. A new CT scan showed the enlargement of the aneurysmal sac (115 mm) due to the persistent Type II endoleak from bronchial arteries (Fig. 3). An endovascular embolization of the target vessels was not feasible due to the impossibility to cannulate the bronchial arteries without direct puncture. A preoperative esophageal endoscopy was performed to exclude the presence of esophageal–aneurysmal fistulas and an open repair with right thoracotomy and aneurysmorraphy of the AARSA was performed to occlude the bronchial side branches and to reduce the compression of the giant aneurysm on the esophagus (Fig. 4, 5). The postoperative course was uneventful and the patient was discharged on the 11th postoperative day.
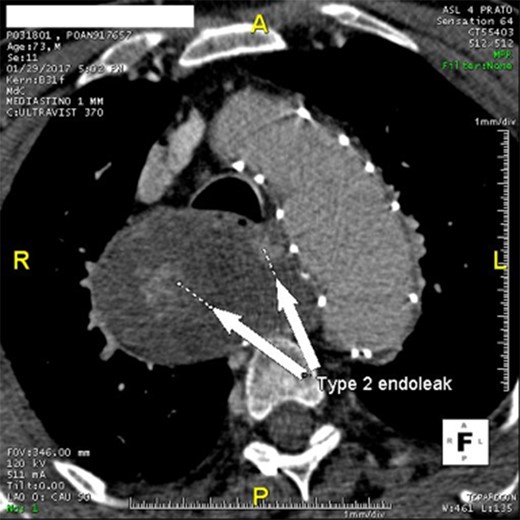
Angio-CT scan at 22 months showing Type II endoleak with significant sac enlargement.
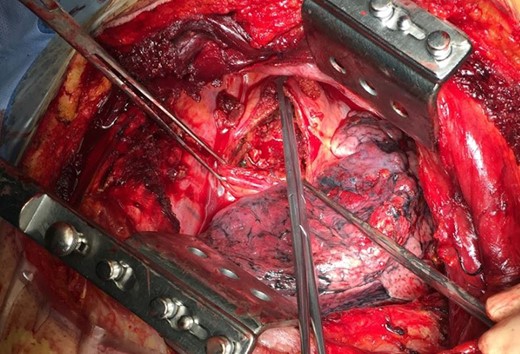
Intraoperative image showing the opened sac with the back bleeding from bronchial vessels.
DISCUSSION
In recent years, an increasing number of reports concerning aneurismal degeneration of aberrant subclavian arteries have been published, mainly due to the increased number of diagnosed asymptomatic lesions and to the evolution of endovascular techniques, which allow to reduce the complications of open surgical repair. In fact, the cumulative perioperative mortality in the open surgery patients is reported up to 12% [6], even if more recent series report a dramatic reduction in perioperative major complications [7]. Nowadays, hybrid surgery is the most used technical solution in elective interventions [8]. It provides low rates of perioperative mortality and morbidity, the resolution of the majority of different anatomical anomalies related to the aberrant arteries and the reduction of spinal cord and cerebral ischemia events and left upper limb malperfusion related to the coverage of the left subclavian artery [9, 10]. On the other hand, mid- and long-term results are not univocal and require further validation, as the hybrid exclusion of AARSA, even if fascinating for its minimal invasiveness, can be complicated by aneurismal reperfusion in the medium- and long-term setting.
In fact, our patient suffered from the development of a persistent Type II endoleak, causing further sac enlargement and the need for an open repair conversion after 22 months of follow-up.
Only two papers [4, 5] previously reported the treatment strategies for Type II endoleak following endovascular or hybrid AARSA repair. In one case, a Type II endoleak from bronchial arteries in an aberrant left subclavian artery aneurysm, previously treated by thoracic endoprosthesis implant, was fixed by endovascular means with coils implanted through a gap between the prosthesis and the subclavian artery. In the other case, such a complication, developed after hybrid repair of AARSA, was treated with aneurysmal sac wrapping and ligation of the patent collateral arteries. In our case, there was no option to gain further access to the aneurysmal sac by endovascular means, so an open approach was mandatory (Fig. 5).
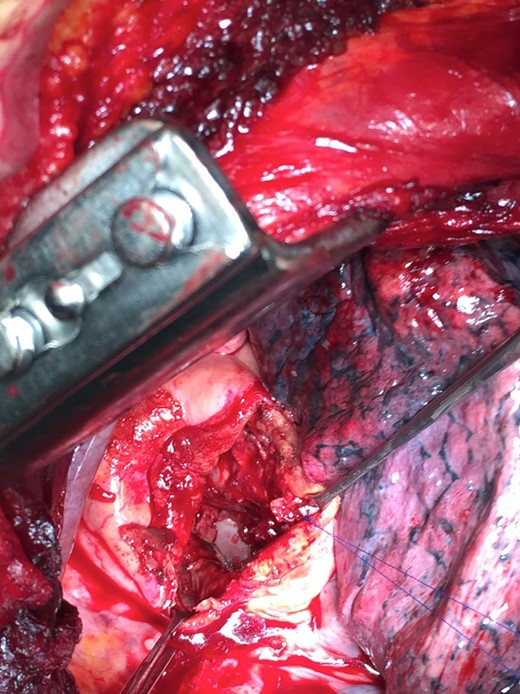
Intraoperative image after intra-sac arterial suture; the endograft is well visible on the bottom.
CONCLUSION
Hybrid surgical treatment in the case of aneurysmatic aberrant subclavian artery is feasible and allows to treat this complex situation with a relatively minimally invasive approach. On the other hand, persistent sac reperfusion after endovascular exclusion can be a dramatic postoperative complication and may undermine the efforts to lower the mortality and morbidity rates using a minimally invasive treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding.



