-
PDF
- Split View
-
Views
-
Cite
Cite
Yuta Koichi, Hayato Ise, Seima Ohira, Daita Kobayashi, Sentaro Nakanishi, Natsuya Ishikawa, Hiroyuki Kamiya, Manual repositioning of lung hernia after minimally invasive cardiac surgery, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz056, https://doi.org/10.1093/jscr/rjz056
Close - Share Icon Share
Abstract
Minimally invasive cardiac surgery has recently become widespread because it has few disadvantages. However, lung hernia has been reported as a rare complication of minimally invasive cardiac surgery (MICS), and normally requiring additional surgical procedures. We describe herein a case of manual repositioning of lung hernia after MICS.
BACKGROUND
Minimally invasive cardiac surgery (MICS) has recently become widespread. The advantages are reductions in trauma, bleeding, wound infection and pain, and faster recovery [1]. However, some cases of lung hernia have been reported, representing a rare complication of MICS [2], and normally requiring additional surgical procedures. We describe herein a case of manual repositioning of lung hernia after MICS.
CASE PRESENTATION
A 51-year-old woman with severe mitral regurgitation presented with New York Heart Association class II heart failure symptoms. Transthoracic echocardiography showed severe mitral regurgitation due to P2 prolapse. She underwent MICS mitral valve repair with folding plasty at P2 and implantation of a semirigid annuloplasty band (CG future band, Medtronic, Inc., Minneapolis, MN, USA). The main skin incision (length, 7 cm) was made below the right breast and the thoracotomy was performed in the fourth intercostal space. The intercostal space was sutured with two pericostal stitches, and skin incision was closed with running subcuticular suture.
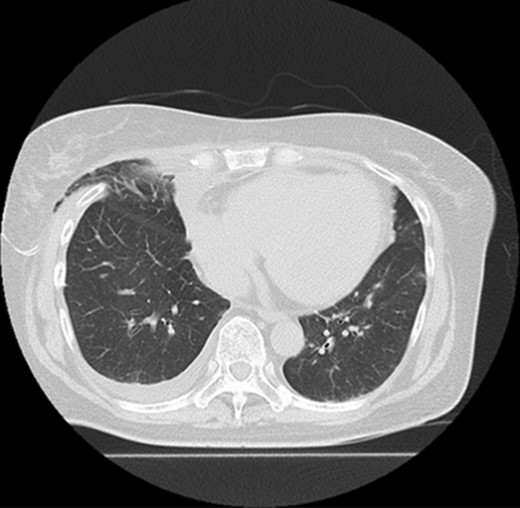
Five days after surgery, she complained of right chest wall pain and discomfort on inspiration. Computed tomography (CT) revealed that part of the right upper lobe of the lung had herniated through the right fourth intercostal space (Fig. 1). Lung hernia was diagnosed. The herniated lung was manually repositioned by compression bandages (Fig. 2). On postoperative Day 11, 6 days after recognition of the herniation, the lung hernia was not apparent on CT. The patient was discharged home without symptoms on postoperative Day 12.

Manual repositioning of the herniated lung by compression bandages.
On follow-up CT at 1 month postoperatively, the upper lobe remained in the thoracic cavity and no sign of lung herniation was apparent (Fig. 3).
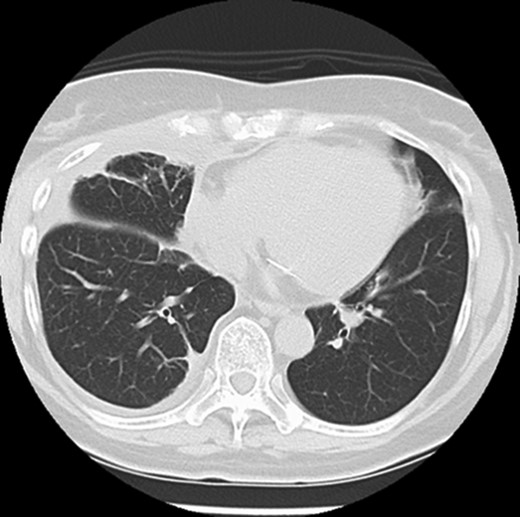
Follow-up CT shows that the lung hernia has returned to the thoracic cavity.
DISCUSSION
Here, we successfully treated a patient with lung hernia after MICS mitral valve surgery by manual repositioning. To the best of our knowledge, this represents the first description of successful manual repositioning of lung hernia.
In 1925, Montgomery and Lutz defined lung hernia as ‘a protrusion of any part of one or both lungs through their boundaries, chiefly the thoracic wall, and usually in a sac of parietal pleura under the skin’ [3]. Only about 300 cases of lung hernia have been reported [4]. Lung herniation is generally classified according to location (cervical, thoracic or diaphragmatic) and cause (congenital or acquired, the latter of which is subdivided into traumatic, spontaneous or pathologic) [5].
Currently, the treatment for lung hernia remains somewhat controversial. In the majority of reported patients, the lung herniates through the intercostal space as a result of trauma or after thoracic surgery [6]. Since symptomatic lung hernia rarely shows spontaneous healing, surgery is considered the standard treatment [7]. The main indications for operation are increasing size, pain, and any signs of impending incarceration [4]. In the present patient, the lung hernia was able to be treated by external manual compression. This experience suggests that lung hernia can potentially be treated without any additional surgery, if diagnosed in the early postoperative phase.
CONCLUSION
We demonstrated that lung hernia can, at least sometimes, be treated by manual repositioning with external mechanical compression. This option may only be possible in the early postoperative phase, so early detection may be crucial to avoid additional surgery in the late phase.
ACKNOWLEDGEMENTS
Not applicable.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No financial support was received in the realization of this case report.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
CONSENT FOR PUBLICATION
We confirm that written informed consent for publication of this case report and the accompanying images was obtained from the patient.
AVAILABILITY OF DATA AND MATERIAL
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.



