-
PDF
- Split View
-
Views
-
Cite
Cite
Timothy Trestrail, Emily K Martin, Neal Bhutiani, Garrett F Mortensen, Vladimir Davidyuk, Gary C Vitale, An unusual presentation of congenital superior mesenteric artery (SMA) syndrome, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz067, https://doi.org/10.1093/jscr/rjz067
Close - Share Icon Share
Abstract
A case of a 39-year-old woman diagnosed with superior mesenteric artery syndrome after a 25-year history of nausea, vomiting, and abdominal pain that began as a teenager and the absence of any significant weight loss illustrates the diagnostic complexity of this entity, particularly among teenagers and young adults who present with these symptoms. The patient underwent multiple upper endoscopies and serologic evaluations before a contrasted CT demonstrated an acutely angled SMA and duodenal compression, prompting the diagnosis of SMA syndrome. This case underscores the importance of including congenital SMA syndrome on the differential in young people without an obvious cause of persistent nausea, vomiting, and abdominal pain.
INTRODUCTION
Superior mesenteric artery (SMA) syndrome is a rare and underdiagnosed cause of small bowel obstruction via compression of the third portion of the duodenum between the aorta and the SMA. This condition, which can be acquired, congenital, or idiopathic, is due to a decreased aortomesenteric angle from a normal range of 38–65 degrees to less than 25 degrees [1]. Acquired cases of SMA syndrome have occurred after significant weight loss or corrective scoliosis surgery, when the protective fat pad cushion between the aorta and SMA was decreased [1]. Congenital causes of SMA syndrome involve short or hypertrophied ligament of Treitz as well as abnormal insertion of the SMA [1, 2]. Overall, this condition is a rare diagnosis due to its low estimated prevalence of 0.1–0.3% and its non-specific presentation of epigastric pain, nausea, and vomiting [3]. Here, we present an unusual case of congenital SMA syndrome in an adult.
CASE REPORT
A 39-year-old woman presented to clinic for evaluation of worsening chronic abdominal pain. The patient had a long-standing (25+ year) history of intermittent abdominal pain, fullness, and distention that began as a teenager. She had been treated with proton pump inhibitors for a diagnosis of gastroesophageal reflux disease (GERD), which only somewhat ameliorated her symptoms. Her only surgical history was an umbilical hernia repair 5 years prior, which resulted in temporary symptom improvement.
Over the course of her disease, the patient had undergone multiple upper endoscopies, which demonstrated a largely dilated duodenum. Serology and hematologic studies were consistently within normal limits. While a diagnosis of SMA syndrome had been considered, it was deemed unlikely given her normal body habitus (body mass index (BMI) = 22) and absence of a history of rapid weight loss.
Immediately prior to presentation, the patient experienced another episode of nausea, abdominal pain, distention, and diarrhea. Again, the patient denied any weight loss and did not exhibit signs or symptoms of systemic infection. Computed tomography (CT) of the abdomen and pelvis with oral and intravenous contrast as well as an upper GI series demonstrated a significantly dilated duodenum with a sharp transition to collapsed small bowel (Fig. 1). CT also demonstrated an acutely angulated SMA with compression of the duodenum between the SMA and the aorta (Fig. 2). Endoscopic evaluation did not demonstrate any evidence of mechanical obstruction of the duodenum.
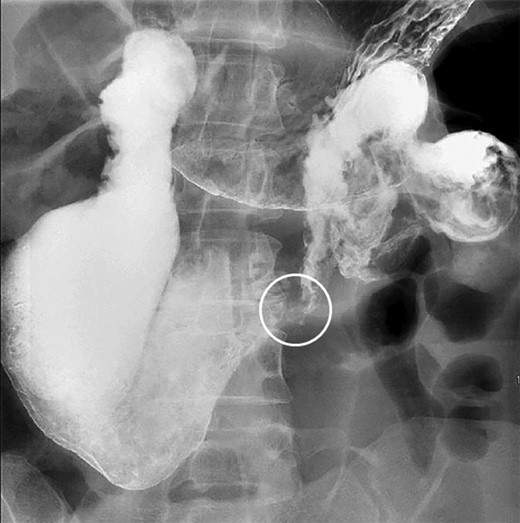
Upper GI demonstrating duodenal dilation with decompressed small bowel distal to a sharp transition point (circle).
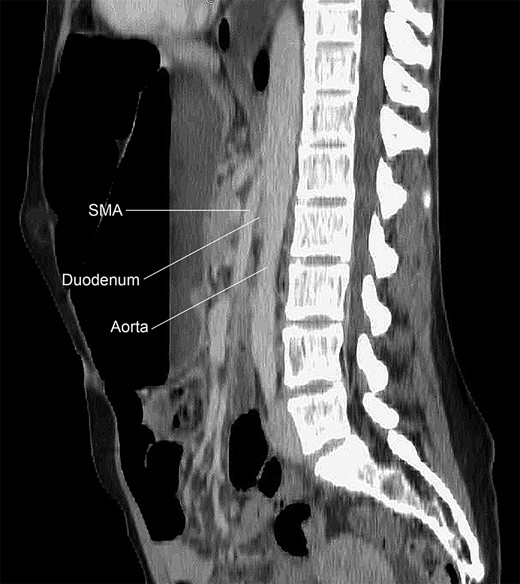
CT of the abdomen and pelvis demonstrating an acutely angulated SMA with compression of the duodenum between the SMA and the aorta.
Given the patient’s clinical picture and the constellation of imaging findings, the patient was diagnosed with SMA syndrome. After an extensive discussion with the patient, she was deemed a poor candidate for non-operative management given her normal BMI in the absence of any history of significant weight fluctuation. She was taken to the operating room for a duodenojejunostomy, which she tolerated well. At last follow-up eight weeks after surgery, the patient reported improvement in her abdominal pain, distention, and diarrhea despite some persistent nocturnal gastrointestinal reflux.
DISCUSSION
SMA syndrome is a rare condition with an estimated incidence of 0.1–0.3% that is most commonly acquired after significant weight loss. This weight loss decreases the mesenteric fat separating the aorta from the SMA, causing the small bowel to become obstructed. Patients with conditions at risk for losing this mesenteric fat and acquiring SMA syndrome include burn or trauma victims, anorexia nervosa, malabsorption conditions, or cachexic states. Congenitally caused SMA syndrome is typically due to an altered ligament of Treitz or an abnormal anatomical placement of the SMA. Approximately 40% of cases of SMA syndrome occur idiopathically [3]. SMA syndrome presents with a variety of imprecise symptoms, including epigastric pain, nausea, vomiting, early satiety, and abdominal distension. This vague symptom profile is associated with a number of other conditions, such as GERD, mesenteric ischemia, biliary colic, and peptic ulcer disease, usually making diagnosis of SMA syndrome one of exclusion. Diagnosis is confirmed with barium swallow and CT or MR angiography [4]. A history of significant weight loss usually increases clinical suspicion for SMA syndrome; however, this can be lacking as observed in this case presentation.
In this case, a 39-year-old lady presented with over 25 years of abdominal pain, fullness, distension, and gastroesophageal reflux (GERD) without any history of significant weight loss. She was initially diagnosed with GERD and treated with proton pump inhibitors. Over the course of these 25 years, she underwent multiple upper endoscopies which showed a dilated duodenum with no mechanical obstruction. A diagnosis of SMA syndrome was made after 25+ years of vague symptomatology when a CT of the abdomen and pelvis demonstrated massive dilation of the duodenum to the iliac crest, acute angulation of the SMA compressing the duodenum, and collapse of the subsequent small bowel.
Initial treatment of SMA syndrome is usually conservative and aimed at relieving small bowel obstruction and its associated symptoms by increasing the fat pad between the SMA and duodenum. Conservative measures may be adequate for disease caused by significant weight loss, and include nasogastric decompression, nutritional support, electrolyte imbalance correction, positional therapy, and prokinetics/reflux medication [5, 6]. Surgical intervention is recommended if conservative measures fail or if chronic disease has caused extensive duodenal dilation with stasis or severe peptic ulcer disease [6]. Current surgical options include duodenojejunostomy, gastrojejunostomy, and Strong’s procedure [7]. In our patient, conservative measures were deemed unlikely to succeed due to her longstanding disease, massive duodenal dilation, normal BMI with fat pad, and 25-year treatment of reflux symptoms without relief.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLOSURES
The authors have nothing to disclose.



