-
PDF
- Split View
-
Views
-
Cite
Cite
Dimosthenis Chrysikos, Theodore Troupis, John Tsiaoussis, Markos Sgantzos, Vasileios Bonatsos, Vasileios Karampelias, Theodoros Piperos, Vasileios Kalles, Panagiotis Theodoropoulos, Dimosthenis Kakaviatos, Ioannis Flessas, Euthumios Nikou, Theodoros Mariolis-Sapsakos, Superior mesenteric artery syndrome: a rare case of upper gastrointestinal obstruction, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz054, https://doi.org/10.1093/jscr/rjz054
Close - Share Icon Share
Abstract
Superior mesenteric artery (SMA) or Wilkie’s syndrome is a rare clinical entity of partial or complete duodenal obstruction. The pathogenic mechanism is an acute angulation of the SMA which leads to compression of the third part of the duodenum between the SMA and the aorta. This is commonly due to loss of fatty tissue as a result of a variety of debilitating conditions. Its treatment is initially conservative and in case of failure, surgical therapy is unavoidable. We present a case of a 68-year-old female patient who presented in our Department with symptoms of dehydration after persistent vomiting for months. After complete radiologic workup, SMA syndrome was diagnosed and was successfully treated operatively. SMA syndrome might be a diagnostic challenge and must be always included in the differential diagnosis of upper gastrointestinal obstruction. Consequently, this paper aims to increase the awareness of a rare entity of duodenal obstruction.
INTRODUCTION
The compression of the anterior duodenal wall by the superior mesenteric artery as a cause of duodenal obstruction was first described by Von Rokitansky in 1861 [1]. The vascular compression of the duodenum through years has been termed as superior mesenteric artery (SMA) syndrome, aortomesenteric duodenal compression syndrome, the cast syndrome or chronic duodenal ileus. In addition, this clinical entity was studied in detail by Wilkie who presented a series of 75 cases in 1921 [2]. Since then, only about 400 cases have been reported in the English literature concerning this unusual cause of upper intestinal obstruction.
In general population, the incidence of SMA syndrome ranges between 0.013% and 0.78% [3].
The pathogenic mechanism of this entity is upper gastrointestinal obstruction caused by partial or complete compression of the third part of the duodenum between the SMA and the aorta [3, 4].
Shedding light to the etiology of the SMA syndrome, one of the consequences of the erect posture of humans is that the superior mesenteric artery leaves the aorta at an acute angle, that ranges from 38° to 65° [4], rather than at a nearly complete right angle as it does in quadrupeds. The main anatomic feature of SMA syndrome is a narrowing of the aorta-SMA angle to <25°, and as a result, the aortomesenteric distance decreases to <10 mm, from normally 10 to 28 mm [4].
Through this vascular angle, between the aorta and the SMA, the third part of the duodenum passes and is thus vulnerable to becoming compressed between the SMA anteriorly and the aorta and vertebral column posteriorly. A number of etiological factors may predispose to this vascular compression of the duodenum.
These factors can be either congenital or acquired. Congenital might be malrotation or paraduodenal hernias.
Acquired conditions develop following surgery or compression associated with severe weight loss.
The first includes spinal surgery, which is the most frequent and surgery-associated rapid weight loss, esophagectomy and abdominal trauma. [4, 5]. SMA syndrome in patients undergoing gastric bypass surgery for the treatment of morbid obesity has a published prevalence of 0.6% [6]. It is much more prevalent than in other patient populations. This can be assumed because the gastric bypass population shares an important risk factor for developing SMA syndrome: rapid weight loss.
The second includes wasting conditions such as AIDS [7], malabsorption, cancer, [8] cerebral palsy and other conditions associated with cachexia; catabolic conditions, burns and eating disorders such as anorexia nervosa [4].
Patients with SMA syndrome may present with signs and symptoms of duodenal upper gastrointestinal obstruction.
CASE REPORT
A 68-year-old Caucasian female patient presented in our Department with abdominal pain and a concomitant 15 kg weight loss over the past 6 months that was unintentional. The pain was mainly located in the epigastrium. She also had symptoms of dehydration, due to persistent postprandial vomiting, during these months. Her medical history included hypertension and diabetes mellitus. Her physical examination was normal and her blood results and an abdominal ultrasound were within normal range.
On admission, a nasogastric tube was inserted and the fluid and electrolyte balance was corrected by parenteric infusion of crystalloid fluids. Two days later, the patient was subjected to gastroscopy which showed mild inflammation of the lower esophageal mucosa and gastritis. The instrument could not pass further from the third part of the duodenum, due to extraluminal pressure on the duodenal wall. Gastrografin swallow confirmed the obstruction of the third part of the duodenum with proximal dilation of the stomach and duodenum (Fig. 1).
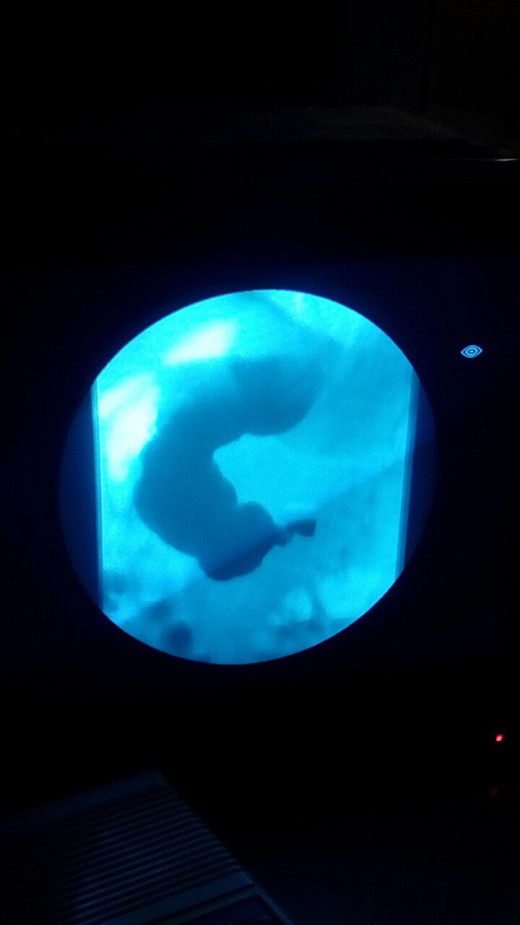
Gastrografin swallow depicting obstruction of the third part of the duodenum with proximal dilation of the stomach and duodenum.
Computerized tomography (CT) scan of the upper and lower abdomen excluded the possibility of a tumor or an annular pancreas to be the cause of the compression of the duodenum. The subsequent CT scan showed an acute angle of 15° (Figs. 2 and 3) between the superior mesenteric artery and the aorta.


Sagittal CT image showing the entrapment of the duodenum between the aorta and the SMA.
Thus, based on the history, the unintentional weight loss may have induced the compression of the third part of the duodenum. In this case, the clinical and the imaging findings of the patient concluded the diagnosis of SMA syndrome.
Following extensive discussion with the patient and her family, she opted for surgery rather than conservative management. She was unwilling to try nasojejunal feeds or total parenteral nutrition (TPN) in the interim.
Therefore, after obtaining informed and written concern, the patient was subjected to laparotomy. The first and second parts of the duodenum were not dilated and hypertrophied as expected, due to acute onset of the syndrome. The duodenum was obstructed at the point where the superior mesenteric artery crossed the third part of the duodenum (Fig. 4). These findings confirmed the diagnosis of SMA syndrome.
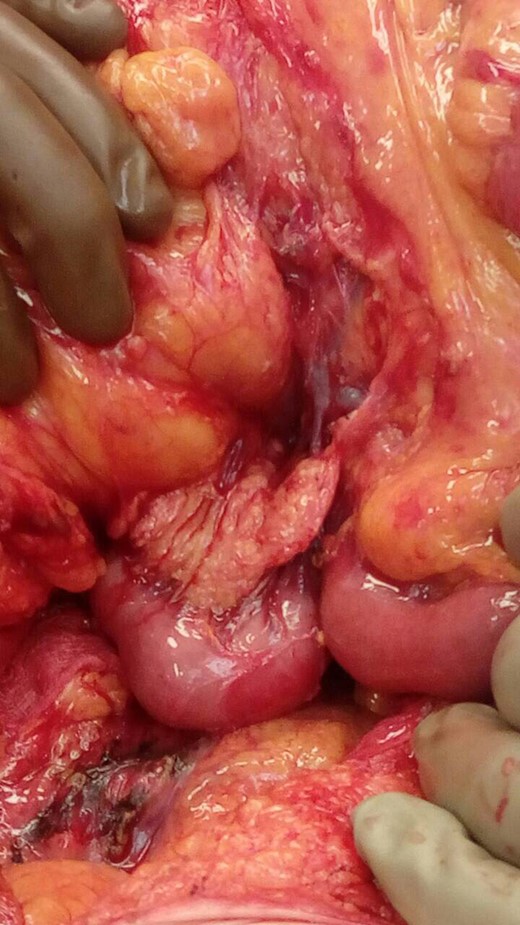
SMA syndrome compression of the third part of the duodenum from SMA.
Due to patient’s hemodynamic instability intraoperatively, Strong’s procedure was performed with lysis of the ligament of Treitz and mobilization of the duodenum (Fig. 4).
The postoperative course was not uncomplicated. There was evidence of gastric outlet obstruction and persistent ileus. The patient had a nasogastric tube that drained about 1.5 l of bilious material per day. She was then subjected to upper gastrointestinal endoscopy to rule out other pathology that may demonstrate external pressure on the third portion of the duodenum.
In addition, repeated difficulties with intravenous line placement, electrolyte abnormalities and falling serum albumin levels indicated that Strong procedure had failed and the patient’s condition necessitated again surgical intervention.
A week after the first operation, she was subjected to new laparotomy where a side to side gastrojejunostomy was performed. The postoperative course was now uncomplicated and she was admitted after 2 weeks.
Afterwards, a barium meal a month later showed postoperatively unobstructed passage of the contents from the stomach to the jejunum.
DISCUSSION
The diagnosis of the SMA syndrome might be a clinical dilemma, due to its insidious presentation. High clinical suspicion is of paramount importance.
Laboratory tests include complete blood count, electrolytes, liver function tests and amylase.
Further radiographic studies to establish the diagnosis must include upper gastrointestinal series, CT scan or CT angiography, magnetic resonance (MR) angiography, conventional angiography, ultrasonography and endoscopy have all been used for diagnosis [2].
Contrast-enhanced CT or MR angiography contributes to diagnosis by measuring the aortomesenteric angle and distance. An aortomesenteric angle of < 22–25° and a distance of < 8 mm correlated well with symptoms of superior mesenteric artery syndrome [9, 10].
However, the existence of SMA syndrome has been doubted; indeed, some investigators have suggested that the SMA syndrome is overdiagnosed because it is confused with other causes of megaduodenum such as diabetes mellitus, collagen vascular conditions or chronic idiopathic intestinal pseudoobstruction. As a result, SMA syndrome necessitates a strict definition and must be substantiated with precise clinical and radiographic criteria.
Treatment consists initially conservative measures. Medical management may be successful in patients with a short history, moderate symptoms and incomplete duodenal obstruction.
In patients who present with acute symptoms of vascular compression, such in our case, a high calorie diet which leads to gain of weight might alleviate or even remove the symptoms. Total parenteric nutrition has also been used but eventually 50–70% of all cases will relapse and may necessitate surgical treatment. The aim of conservative approach with jejunal or parenteral nutrition is the restoration of the aortomesenteric adipose tissue that in the normal individual displaces the SMA anteriorly away from the aorta so avoiding duodenal compression.
In our case, the patient refused conservative treatment, which may include TPN for at least a week. Due to acute deterioration of chronic symptoms and the laboratory values (electrolytes, albumin), we immediately proceeded with the surgical treatment.
Intraoperatively, there was an obvious compression of the third part of the duodenum and the patient was hemodynamically unstable during the operation. We decided to perform a less conventional surgical procedure, avoiding anastomosis in view of the patient’s high risk for surgical intervention. Initially, after mobilization of the duodenojejunal flexure, an attempt was made at duodenal derotation, by dividing the ligament of Treitz (Strong’s procedure). This surgical option has a failure rate of 25% [4].
Other operative modalities may include duodenojejunostomy, relocation of the duodenojejunal junction, gastroenterostomy, duodenal anterior replacement and Billroth II gastrectomy. Duodenojejunostomy was first introduced by Starley in 1910 and, over the years, it is the most frequent treatment as it is performed in 69% of surgical treated cases with excellent results. Nowadays, duodenojejunostomy is the operation of choice to relieve the obstruction, with a success rate up to 90%. In addition, advances in laparoscopic surgery have seen laparoscopic Strong procedures and laparoscopic duodenojejunostomy reported by several centers [11].
However, in some cases, the decision of the operative strategy can only be determined in the operating theater.
In our case, at first laparotomy due to severe hemodynamic instability, we were very cautious to perform any anastomosis. After the second laparotomy, the decision to perform gastrojejunostomy rather than duodenojejunostomy was made after consideration of several points. We wanted to avoid a potentially higher risk of anastomotic leak after relocation of the duodenojejunal junction in front of the vascular compression. It was obvious that Strong procedure has failed.
The stomach was also more proximal anatomically and now decompressed following nasogastric tube aspiration and, therefore, chosen for anastomosis with the jejunum. The gastrojejunostomy was also decided because of gastric distention which has caused gastroparesis and delayed emptying of the stomach.
However, gastrojejunostomy may have the risk of peptic stomal ulceration and other postoperative complications like blind loop syndrome and recurrence of symptoms due to non-decompression of the duodenum.
To conclude, SMA syndrome necessitates high clinical suspicion especially in patients with severe weight loss and symptoms of gastric distension followed by persistent vomiting. Multydisciplinary approach provides an accurate diagnosis and treatment.
Finally, we would like to emphasize the difficulty of achieving an accurate diagnosis of SMA. Failure of conservative treatment leads to surgical intervention. Duodenojejunostomy is the operation of choice; however, the surgical approach may be undertaken intraoperatively. It was Strong procedure that led to an unsuccessful first laparotomy and then to a second successful gastrojejunostomy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
All authors declare that are no funding requirements.



