-
PDF
- Split View
-
Views
-
Cite
Cite
Zdravko Štor, Jurij Hanžel, Ileal leiomyosarcoma presenting with intussusception, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz052, https://doi.org/10.1093/jscr/rjz052
Close - Share Icon Share
Abstract
Intussusception is a rare cause of small bowel obstruction in adults, up to 30% of cases are caused by small bowel malignancy. Intestinal leiomyosarcoma is an extremely rare malignant mesenchymal tumour. An 80-year-old male presented with small bowel obstruction. Abdominal ultrasonography and a subsequent CT scan showed small bowel obstruction due to ileo-ileal intussusception. The patient underwent an emergency exploratory laparotomy, which confirmed prior findings on imaging. The affected segment of the ileum was resected and a primary entero-enteral anastomosis was created. Histopathological analysis revealed a 4.8 cm leiomyosarcoma. The patient remains without evidence of disease 12 months after initial presentation. Radical surgical resection remains the treatment of choice for leiomyosarcoma, with no convincing evidence supporting adjuvant treatment. Tumours smaller than 5 cm appear to have a more favourable prognosis.
INTRODUCTION
Small bowel obstruction is responsible for about 20% of presentations with acute abdomen. A significant percentage of those patients (18–57%) requires surgical intervention. Small bowel obstruction can be difficult to recognize preoperatively and is associated with significant mortality [1].
Among the different causes of small bowel obstruction 60% are due to postoperative adhesions, followed by malignancy, inflammatory bowel disease, and hernias [2]. Malignant tumours of the small bowel accounts for 2% of all gastrointestinal tumours and 1% of gastrointestinal tumour-related deaths [3]. The diagnosis is difficult, because their symptoms and signs are nonspecific at presentation. Therefore, they are usually discovered at an advanced stage and often require surgical intervention due to acute complications [4]. We present a case of small bowel obstruction due to intussusception caused by an ileal leiomyosarcoma.
CASE REPORT
An 80-year-old male patient was referred to our department due to constipation and abdominal pain. The patient had a three-week history of persistent abdominal pain and one-week history of constipation, but he was still able to pass flatus.
He had arterial hypertension and dyslipidaemia. Prior to this admission he had undergone oesophagogastroduodenoscopy and colonoscopy due to abdominal pain and anaemia. Oesophagogastroduodenoscopy showed erosive gastritis, colonoscopy showed diverticulosis of the sigmoid colon. Laboratory tests showed anaemia (haemoglobin 9 g/dL) and a mildly elevated C-reactive protein (68 mg/L). A plain abdominal X-ray showed air-fluid levels of the small intestine and abdominal ultrasonography confirmed intussusception of the small intestine and developing small bowel obstruction. Computerized tomography showed small bowel obstruction with dilated small bowel loops due to ileo-ileal intussusception (Fig. 1).

Abdominal CT scan ileo-ileal intussusception with a target sign (arrow).
The patient was scheduled for emergency exploratory laparotomy. A small median laparotomy was performed and during exploration of the abdominal cavity, we discovered dilated small bowel loops with an invaginated segment. We explored the entire abdominal cavity, but we did not find any other pathology. Liver and other peritoneal surfaces were without evident pathology. We resected the invaginated segment of the ileum and performed primary entero-enteral anastomosis. The postoperative course was uneventful and the patient was discharged on the eighth postoperative day.
Histopathological examination revealed a 4.8 cm leiomyosarcoma of the terminal ileum (Figs2and3). The tumour involved the full thickness of the ileum. It was located 4.5 cm from the intestinal and 1.5 cm from the radial resection margin. One adjacent lymph node was retrieved, but contained no tumour cells. Immunophenotyping for CD 117 (c-kit) and DOG1 was negative and positive for desmin and caldesmon was positive. The proliferation index Ki67 was 60%. Following a multidisciplinary team meeting, no adjuvant therapy was indicated and the patient remains without evidence of disease 12 months since initial presentation.
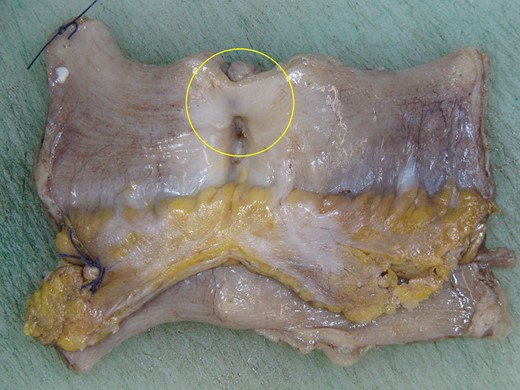
Gross photograph of resection specimen showing the ileal leiomyosarcoma (yellow circle).
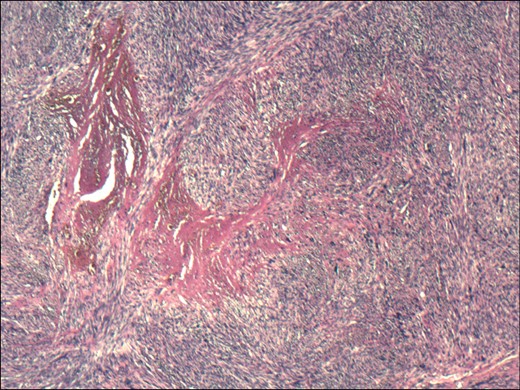
Haematoxylin and eosin stained section showing a spindle-celled tumour with pleomorphic nuclei and pronounced mitotic activity.
DISCUSSION
Intussusception occurs when one segment of the gastrointestinal tract and its mesentery (intussusceptum) invaginate into the lumen of an adjacent distal segment (intussuscipiens), which may cause luminal obstruction and ischaemia. It is rare in adults and accounts for less than 5% of bowel obstruction, with the small bowel as the commonest site [5]. Lesions associated with small bowel intussusception include adhesions, strictures, inflammatory fibrous polyps, lipomas, leiomyomas, haemangiomas, Meckel’s diverticula, metastatic lesions (from melanoma, breast and lung), gastrointestinal stromal tumours, leiomyosarcomas, malignant fibrous histiocytomas, lymphomas, neuroendocrine neoplasms, adenocarcinomas, and Peutz–Jeghers polyps. The following conditions have been associated with small bowel intussusception: IgA vasculitis (formerly Henoch–Schönlein purpura), coeliac disease, Crohn’s disease, lymphadenitis and human immunodeficiency virus related infections or malignancies. It is estimated that 20–30% of small bowel intussusceptions in adults are caused by malignancy [5, 6]. For this reason, primary resection without attempting reduction is the preferred treatment in adults.
Primary malignancies of the small bowel are rare. The incidence rate of primary small bowel tumours in the USA is 22.7 per million, with neuroendocrine neoplasms as the commonest histological type, followed by adenocarcinoma, lymphoma and stromal tumours [7]. Most patients have nonspecific clinical symptoms and signs, such as abdominal pain, weight loss and anaemia. In a study by Han et al., the most frequent symptoms were abdominal pain (67.4%), abdominal mass (31.2%), bowel obstruction (24.1%), haematochezia (21.3%), jaundice (16.3%), fever (14.2%), bowel perforation and peritonitis (5.7%), gastrointestinal bleeding (5.0%), and intraabdominal bleeding (1.4%) [4].
Morphologically, leiomyosarcoma is a spindle-celled tumour resembling a gastrointestinal stromal tumour. The two entities are best distinguished with immunochemistry with leiomyosarcomas positive for smooth muscle cell markers (smooth muscle actin, desmin, caldesmon) and negative for c-kit and DOG1, as in our case. The tools to definitively distinguish the two were only developed in the late 1990s [8]. Gastrointestinal leiomyosarcomas are exceedingly rare, with a recent literature review highlighting only 76 published cases, 30 of which were in the small bowel [9]. Ileum was the second most common site of the tumour in the small intestine after the duodenum.
Surgical resection with negative margins is the gold standard of treatment, with no proven benefit of adjuvant therapy. In metastatic disease, first-line therapy with doxorubicin and olaratumab is advised for patients with excellent performance status, while in patients with comorbidities liposomal doxorubicine or a gemcitabine-based regimen can be considered. Trabectedin has recently been approved as a second-line agent [10]. The rarity of the tumour precludes a comprehensive survival analysis stratified by tumour site. It appears that a tumour size below 5 cm and a lower number of mitoses are associated with a better prognosis, although these findings are not consistent between studies.
Conflict of Interest statement
None declared.
References
- small bowel obstruction
- computed tomography
- leiomyosarcoma
- immunologic adjuvants
- pharmaceutical adjuvants
- adult
- anastomosis, surgical
- intestines
- intussusception
- diagnostic imaging
- ileum
- neoplasms
- malignant neoplasm of small intestine
- soft tissue sarcomas
- abdominal ultrasonography
- laparotomy, exploratory
- ileoileal intussusception
- excision



