-
PDF
- Split View
-
Views
-
Cite
Cite
Tetyana Kelly, Paul Liebenberg, Adrian Cohen, A rare case report of small bowel obstruction following colonoscopy, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz049, https://doi.org/10.1093/jscr/rjz049
Close - Share Icon Share
Abstract
Bowel obstruction following colonoscopy is very rare. We present a case of a 53-year-old female who underwent elective colonoscopy and haemorrhoidectomy. She developed generalized abdominal pain and distension with CT findings suggestive of small bowel obstruction. The patient underwent an emergency laparotomy, which revealed ischemic small bowel which had internally herniated through an adhesional band around cecum. Bowel ischemia recovered following adhesiolysis and the patient was spared from having a bowel resection. She recovered well after 2 days in ICU. We present a very rare case of small bowel obstruction following routine colonoscopy.
INTRODUCTION
Bowel obstruction following colonoscopy is very rare. The recurrent literature describes only a handful of cases. We present a rare case of a 53-year-old female who developed bowel obstruction following elective colonoscopy, who gave consent to be included in this case report. The patient required an emergency laparotomy, to prevent worsening of bowel ischemia. She was spared from having a bowel resection following adhesiolysis and recovered well after a few days in ICU. We present a very rare case of adhesional small bowel obstruction following routine colonoscopy.
CASE REPORT
A usually healthy 53-year-old female presented for an elective colonoscopy and haemorrhoidectomy. This was on the background of change in bowel habit and hemorrhoids, which developed after two normal vaginal deliveries. Her past history included appendicectomy aged 8 years of age, a few mild bouts of diverticulitis and constipation with chronic laxative use.
Colonoscopy revealed melanosis coli, diverticulosis and grade four hemorrhoids. She was admitted overnight following haemorrhoidectomy. The following morning she complained of abdominal pain, which she described similar to diverticulitis, and she was tender on exam. To rule out perforation, a plain film abdomen was performed. Findings were suggestive of gaseous distension following colonoscopic air insufflation without evidence of free gas (Fig. 1). Watchful waiting approach was adopted, however the patient deteriorated further during the course of the day. She had a vasovagal episode with tachycardia (134 bpm) and hypotension (67/47 mmHg). A venous blood gas revealed lactate level of 7 mmol/l. She underwent an urgent CT with findings suggestive of pericaecal internal hernia with the ileal loops located in the right paracolic gutter demonstrating features of ischemia (Fig. 2). There was moderate amount of free fluid, but no free gas to suggest perforation (Fig. 3). She was taken to theater that day for emergency laparotomy. The intraoperative findings included two litres of bloodstained fluid and floppy cecum with a band of adhesion to its own mesenteric base, probably adhesional having developed after the appendicectomy. This band has created a window through which three quarters of her small bowel had herniated and became strangulated. The bowel looked very ischemic, but not necrosed. The surgeons divided the adhesion, untwisted the small bowel and waited 20 minutes to allow sufficient time for bowel ischemia to recover. Fortunately, she did not require any bowel resection.

Plain film of abdomen showing colonic gaseous distension following colonoscopy.

CT coronal view showing pericaecal internal hernia of ileal loops demonstrating features of ischemia.
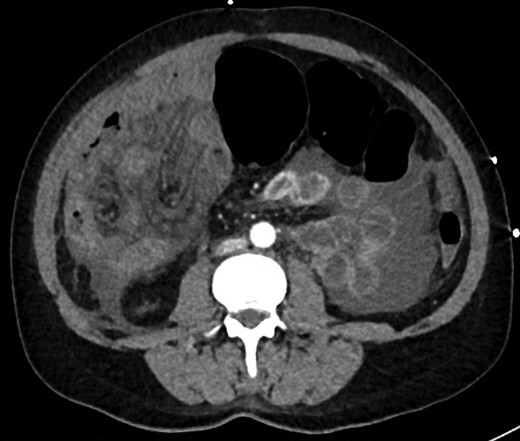
CT axial view showing dilated colon, internal hernia with ischemic small bowel loops, free fluid, but no free gas.
DISCUSSION
Only a handful of previous similar case reports have been described in the literature [1–4]. Most of them occurred in previously operated abdomens (appendectomy, hysterectomy, bowel resection, colpopexy). Malki et al. [2] described patients with small bowel obstruction presenting 24–72 hours following colonoscopy and improving while treated conservatively, Hunter et al. [1] described a patient who underwent resection of non-viable bowel 8 hours following colonoscopy. In our case, the patient remained in hospital due to concurrent operation. This allowed us to avoid delay in diagnosis and save ischemic bowel promptly.
Hunter et al. [1] suggested that extensive insufflation and manipulation of bowel might be a potential cause for causing internal herniation through previous adhesional bands. The authors recommend using torque steering, avoiding extensive insufflation and pushing to maintain straight colonoscope and short colon.
In conclusion, this case demonstrates a very rare cause of small bowel obstruction from strangulated internal hernia following routine colonoscopy.
Conflict of Interest statement
The authors have no conflicts of interest or affiliations to disclose.
Funding
None.
References
Author notes
The corresponding author is not a recipient of a research scholarship.



