-
PDF
- Split View
-
Views
-
Cite
Cite
Kota Sahara, Atsushi Ishibe, Taichi Yabuno, Hiroki Kondo, Gakuryu Nakayama, Shota Yasuda, Takahiro Nishida, Jun Watanabe, Yasuko Uranaka, Hirotoshi Akiyama, Akira Sugita, Itaru Endo, Acute iliac arterial thrombosis during laparoscopic abdominoperineal resection, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz020, https://doi.org/10.1093/jscr/rjz020
Close - Share Icon Share
Abstract
Acute iliac arterial thrombosis during surgery is very rare complication. There were few reports on this complication relative to gastroenterological surgery, and the risk has not been recognized.
A 70-year-old man, diagnosed with a rectal cancer (adenocarcinoma of rectum) with known history heavy cigarette smoking with no known history of peripheral vascular disease underwent a laparoscopic abdominoperineal resection. He presented severe pain in the left leg in the recovery room. A computed tomography (CT) scan revealed the complete obstruction of the left common iliac artery. A successful revasculization was achieved through a thrombotectomy and percutaneous transluminal angioplasty with a stent immediately after the diagnosis. The pain in the left leg disappeared immediately after the revasculization.
An acute arterial thrombosis is a potential complication of the laparoscopic colorectal surgery with the lithotomy position.
INTRODUCTION
Acute compartment syndrome (ACS) in the lower extremities causing peroneal nerve dysfunction and deep vein thrombosis (DVT) is widely recognized as a complication during the surgery with the lithotomy position [1]. In comparison to ACS, acute arterial thrombosis during the surgery is extremely rare complication. We report a novel case which had acute iliac arterial thrombosis through the laparoscopic abdominoperineal resection and was rescued with prompt diagnosis and emergent thrombectomy.
CASE REPORT
A 70-year-old man underwent a colonoscopy after having episodes of bright red stool per rectum and diarrhea. A lower rectal cancer was diagnosed based on a histology obtained through a biopsy of the rectal lesions (Rb, T2N0M0 cStageI (UICC Classification, 7th ed)). The past medical history was notable for hypertension untreated and smoking 50 pack year. His height was 173 cm, and weight was 73 kg with body mass index of 24.4. The creatinine clearance was 87 ml/min. Although the preoperative history talking failed to recognize the symptoms of intermittent claudication and sensory impairment of his lower extremities, a preoperative contrast enhanced computed tomography (CT) scan demonstrated a significant stenosis in bilateral external iliac artery due to arteriosclerosis obliterans (ASO) (Fig. 1) and occlusions of bilateral internal iliac artery. There was no coagulation abnormality in his blood test or atrial fibrillation on an electrocardiogram.
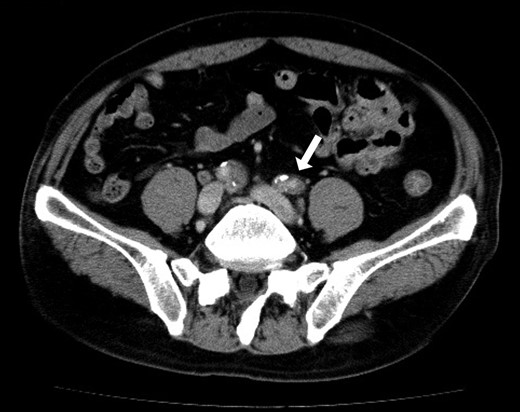
Preoperative abdominal CT showed bilateral iliac arterial stenosis to 5 mm diameter with calcification (the arrows). Internal iliac arteries had been obstructed bilaterally.
He underwent an elective laparoscopic abdominoperineal resection with a lithotomy position. There was no vascular injury or compression with laparoscopic forceps as far as we were able to recognize retrospectively based on the laparoscopic video and the memory. The duration of surgery was 4 hours and 48 minutes. Blood loss was estimated 100 ml, the urine volume was only 50 ml during the operation. In-out balance during operation divided body weight and time of operation was 6.38 ml/kg/h. The patient reported a severe pain in the left leg, when he woke up post-operatively. The left leg was pale and cold, associating sensory abnormality and motor dysfunction; left pedal and popliteal pulses were absent. A CT scan revealed the contrast interruption of left common iliac artery (CIA) over 11.5 cm and suspected to be due to an arterial thrombosis (Fig. 2). Under the local anesthetic technique, the left femoral artery was exposed and performed thrombectomy with a 5Fr Fogarty catheter. After a new clot was removed, aortography revealed persistent stenosis in left iliac artery. Consequently, a Percutaneous transluminal angioplasty (PTA) with stent (Express LD 8 × 37 mm) was added (Fig. 3) via left femoral artery. Blood perfusion in his left leg improved markedly immediately post PTA. The patient was transferred to the intensive care unit for two days due to the complications with a rhabdomyolysis (creatinine phosphokinase up to 23 598 IU/l). The patient started walking 5 days post-surgery, however, the patient was left with the numbness in his left lower leg. A heparinization had been commenced on the postoperative day 1, then this was switched to the cilostazol prior to the discharge for home. We note that the patient continued reporting the left lower leg numbness even one year past the surgery.
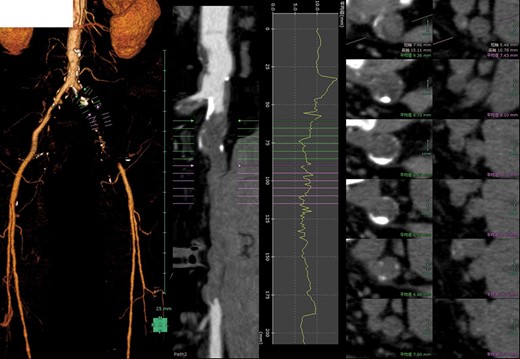
Postoperative 3D-contrast enhanced CT revealed the complete obstruction of left common iliac artery (CIA). The sagittal section through the left iliac artery and the graph of left CIA’s internal diameter showed significant stenosis.
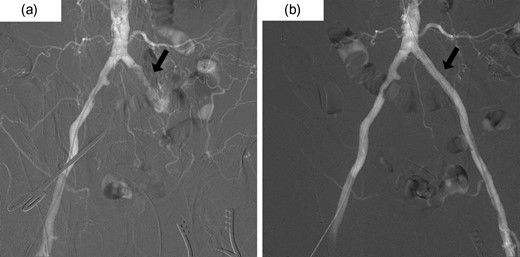
(a) Pre-intervention aortography demonstrating occlusion of the left CIA and the development of collateral circulation in left pelvic cavity. (b) Post-intervention aortography showing improvement of occlusion by a percutaneous transluminal angioplasty (PTA) with stent.
DISCUSSION
Causes of acute limb ischemia include acute thrombosis of limb artery, embolism from the heart or a diseased artery, dissection, and trauma [2]. In our case, the thrombosis was presumed to associate with acute limb ischemia according to the past history and operative findings without traumatic procedure. No article elaborated the incidence of iliac arterial thrombosis during the surgery but, to the best of our knowledge, there are only eight cases reporting the intraoperative acute limb ischemia in terms of pelvic surgeries except this case (Table1) [3–8]. Of note, this is the first case with acute limb ischemia during a laparoscopic gastroenterological surgery.
Summary of reported nine cases of acute limb ischemia during surgical procedure
| Year . | Age . | Sex . | Risk factors for ASO . | Primary disease . | Approach . | Cause of acute limb ischemia . | Location of arterial thrombosis . |
|---|---|---|---|---|---|---|---|
| 1996 3) | 63 | F | DM, HT | Endometrial cancer | Open | Thrombosis | Right, femoral |
| 19 963) | 40 | F | DM | Cervix cancer | Open | Thrombosis | Left, external |
| 19 963) | 69 | F | None | Ovarian cancer | Open | Thrombosis | Right, femoral |
| 20 004) | 46 | M | Smoking, DM, HT, HC | Bladder tumor | Open | Thrombosis | Right, external |
| 20 025) | 68 | F | HT, HC | Rectal cancer | Open | Thrombosis | Bilateral, femoral |
| 20 086) | 34 | F | None | Endometrial cancer | Open | Compartment syndrome | — |
| 20 097) | 13 | F | None | Unicornuate uterus | lap | Trauma | — |
| 20 178) | 37 | F | None | Cervical cancer | lap | Compartment syndrome | — |
| Present case | 70 | M | Smoking, HC | Rectal cancer | lap | Thrombosis | Left, common |
| Year . | Age . | Sex . | Risk factors for ASO . | Primary disease . | Approach . | Cause of acute limb ischemia . | Location of arterial thrombosis . |
|---|---|---|---|---|---|---|---|
| 1996 3) | 63 | F | DM, HT | Endometrial cancer | Open | Thrombosis | Right, femoral |
| 19 963) | 40 | F | DM | Cervix cancer | Open | Thrombosis | Left, external |
| 19 963) | 69 | F | None | Ovarian cancer | Open | Thrombosis | Right, femoral |
| 20 004) | 46 | M | Smoking, DM, HT, HC | Bladder tumor | Open | Thrombosis | Right, external |
| 20 025) | 68 | F | HT, HC | Rectal cancer | Open | Thrombosis | Bilateral, femoral |
| 20 086) | 34 | F | None | Endometrial cancer | Open | Compartment syndrome | — |
| 20 097) | 13 | F | None | Unicornuate uterus | lap | Trauma | — |
| 20 178) | 37 | F | None | Cervical cancer | lap | Compartment syndrome | — |
| Present case | 70 | M | Smoking, HC | Rectal cancer | lap | Thrombosis | Left, common |
ASO, arteriosclerosis obliterans; DM, diabetes mellitus; HT, hypertension; HC, hypercholesterolemia; lap, laparoscopic; -: not available
Summary of reported nine cases of acute limb ischemia during surgical procedure
| Year . | Age . | Sex . | Risk factors for ASO . | Primary disease . | Approach . | Cause of acute limb ischemia . | Location of arterial thrombosis . |
|---|---|---|---|---|---|---|---|
| 1996 3) | 63 | F | DM, HT | Endometrial cancer | Open | Thrombosis | Right, femoral |
| 19 963) | 40 | F | DM | Cervix cancer | Open | Thrombosis | Left, external |
| 19 963) | 69 | F | None | Ovarian cancer | Open | Thrombosis | Right, femoral |
| 20 004) | 46 | M | Smoking, DM, HT, HC | Bladder tumor | Open | Thrombosis | Right, external |
| 20 025) | 68 | F | HT, HC | Rectal cancer | Open | Thrombosis | Bilateral, femoral |
| 20 086) | 34 | F | None | Endometrial cancer | Open | Compartment syndrome | — |
| 20 097) | 13 | F | None | Unicornuate uterus | lap | Trauma | — |
| 20 178) | 37 | F | None | Cervical cancer | lap | Compartment syndrome | — |
| Present case | 70 | M | Smoking, HC | Rectal cancer | lap | Thrombosis | Left, common |
| Year . | Age . | Sex . | Risk factors for ASO . | Primary disease . | Approach . | Cause of acute limb ischemia . | Location of arterial thrombosis . |
|---|---|---|---|---|---|---|---|
| 1996 3) | 63 | F | DM, HT | Endometrial cancer | Open | Thrombosis | Right, femoral |
| 19 963) | 40 | F | DM | Cervix cancer | Open | Thrombosis | Left, external |
| 19 963) | 69 | F | None | Ovarian cancer | Open | Thrombosis | Right, femoral |
| 20 004) | 46 | M | Smoking, DM, HT, HC | Bladder tumor | Open | Thrombosis | Right, external |
| 20 025) | 68 | F | HT, HC | Rectal cancer | Open | Thrombosis | Bilateral, femoral |
| 20 086) | 34 | F | None | Endometrial cancer | Open | Compartment syndrome | — |
| 20 097) | 13 | F | None | Unicornuate uterus | lap | Trauma | — |
| 20 178) | 37 | F | None | Cervical cancer | lap | Compartment syndrome | — |
| Present case | 70 | M | Smoking, HC | Rectal cancer | lap | Thrombosis | Left, common |
ASO, arteriosclerosis obliterans; DM, diabetes mellitus; HT, hypertension; HC, hypercholesterolemia; lap, laparoscopic; -: not available
In present case, there seemed to be multiple risk factors for arterial thrombosis which were ASO, head-down lithotomy position, intravascular dehydration and hypercoagulopathy. ASO was retrospectively suspected from the iliac arterial calcification on the CT and might be responsible mainly. Additionally, it indicated background ASO that he had two risk factors of ASO, smoking and hypertension, among the risk factors such as smoking, diabetes, hypertension and hypercholesterolemia [9]. In regards of the body position during operation, Horgan et al. elaborated the addition of 15°head-down tilt led to an immediate and significant drop in lower limb perfusion with lithotomy position [10]. This fact could suggest that laparoscopic rectal surgery often using deeply head-down lithotomy position tends to decrease the perfusion in lower limb compared with open approach. Furthermore, intravascular dehydration was highly suspected by clinical factors, urine volume, in-out balance described above and systolic blood pressure remaining about 90 mmHg during the surgical procedure. Hypercoagulopathy associated with the concurrent and active cancer may have contributed the vascular complications.
Table 1 summarized nine reported cases of acute limb ischemia during surgical procedure Including present case. Six patients were diagnosed as cancer of ninth patients caused by thrombosis, and it suggests the association between cancer and thrombotic ischemia. Remarkably, patients without risk factor of ASO had experienced acute limb ischemia owing to intraoperative injuries or compartment syndrome.
We failed to predict the risk of arterial thrombus complication at a stage of preoperative evaluation, while the prompt diagnosis and surgical intervention for arterial thrombus prevented from the potentially worse outcomes, such as total limb necrosis requiring amputation. As an alternative evaluation, an Ankle Brachial Pressure Index (ABI) may have been valuable measurement during the preoperative evaluation. Moreover, the perioperative monitoring of pedal blood pressure by intra-arterial cannulation or pulse oximeter on lower limbs may have been convenient and useful if routinely performed for high risk patients. This is a relatively simple procedure and provide an immediate reaction when there is decreased flow to the foot. An acute arterial thrombosis is a potential complication of the colorectal surgery with lithotomy position, especially performed laparoscopically. Surgeons should recognize multiple risks of arterial thrombosis and minimize the patient’s complications by early detection and intervention.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The all authors declare that they have no competing interests.
FUNDING
No grant support of funding from public institution or private enterprises was received.
REFERENCES
- peripheral vascular diseases
- stents
- computed tomography
- balloon angioplasty
- arterial thrombosis
- adenocarcinoma
- colorectal surgery
- ilium
- laparoscopy
- pain
- postoperative anesthesia care unit
- surgical procedures, operative
- diagnosis
- leg
- rectum
- surgery specialty
- rectal carcinoma
- common iliac artery
- lithotomy position
- laparoscopic abdominoperineal resection of the rectum
- cigarette smoking



