-
PDF
- Split View
-
Views
-
Cite
Cite
Turki Khaled Aljohani, Abdullah Mohammed Alshamrani, Ali Mohammed Alzahrani, Rami Abdulrahman Sairafi, A rare case of small bowel obstruction secondary to activated charcoal administration, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz033, https://doi.org/10.1093/jscr/rjz033
Close - Share Icon Share
Abstract
Intestinal obstruction is a rare complication of the administration of activated charcoal. We describe a 22-year-old patient who had received multiple-dose activated charcoal for carbamazepine intoxication. The patient presented with sudden-onset abdominal pain after discharge from the emergency room, and abdominal imaging examinations revealed findings consistent with small bowel obstruction. Laparoscopic-assisted exploration of the abdomen was offered, and a hard obstructing charcoal mass was found in the small bowel. Clinicians should be aware of the rare occurrence of gastrointestinal complication or obstruction following the administration of multiple-dose activated charcoal, especially in patients who ingested a drug that is potentially antiperistaltic.
INTRODUCTION
Activated charcoal has been used since the 1970s [1], and it is the most commonly employed method of gastrointestinal evacuation [2]. It is usually administered as a single dose, and it is thought that its large surface area allows for the adsorption of many drugs and toxins in the gastrointestinal tract, decreasing their absorption into the general circulation. While activated charcoal is generally safe, the compound is not risk-free. Adverse events, such as vomiting and aspiration into the respiratory system have been associated with its administration, precluding the routine use of the compound in clinical practice [3]. Additionally, multi-dose activated charcoal administration is reported to be more likely to cause intestinal obstruction and perforation necessitating a surgical intervention.
A handful of reports describe small bowel obstruction occurring following the administration of activated charcoal [2, 4]. We present the case of a patient who developed small bowel obstruction following the administration of activated charcoal for carbamazepine intoxication.
CASE PRESENTATION
A 22-year-old male, university student presented with a history of sudden-onset abdominal pain of 1-day duration. The pain was colicky, constant and diffuse. It did not radiate and had no aggravating or relieving factor, but it was associated with vomiting. The patient also reported having no bowel movement for one day. He presented to emergency department 2 days ago complain of ataxia and slurred speech, due to a carbamazepine overdose, for which he admitted under neurology and received activated charcoal 150 g, through a nasogastric tube, over 24 h. He had charcoal-stained vomiting during admission; however, his clinical condition improved, and kept for observation then he was subsequently discharged.
The patient had no history of fever, weight loss, fatigue, night sweats or previous episodes of abdominal pain. His medical history was remarkable for dilated cardiomyopathy, for which he was receiving medications. He also had a history of sleeve gastrectomy, which had been performed four years earlier. His family history was unremarkable.
On examination, the patient was conscious, alert, and oriented, but he complained of mild pain. His vital signs were as follows: heart rate, 83 beats per minute; respiratory rate, 22 cycles per minute; blood pressure, 125/83 mmHg; temperature, 37.2°C; and oxygen saturation, 98%. A chest and lung examination was unremarkable. Similarly, a heart examination showed normal first and second heart sounds with no added sounds. His abdomen was soft and distended, with mild generalized tenderness; however, no sign of rigidity or guarding was observed. A digital rectal examination revealed an empty rectum with no blood or stool.
Blood was drawn for a complete blood count, urea and electrolytes, liver function test, coagulation profile, serum glucose level, carcinoembryonic antigen and cancer antigen, and the results were all within normal limits. An initial abdominal X-ray showed multiple air fluid levels and a dilated bowel (Fig. 1A and B). A computed tomography scan of the abdomen and pelvis showed small bowel obstruction to the level of the proximal ileal loops, with a transition point between the dilated proximal loops and the collapsed terminal ileal loops (Fig. 2A and B).
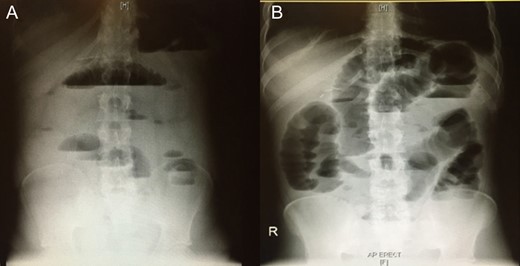
Initial abdominal x-ray showing multiple air–fluid levels (A) and a dilated bowel (B).
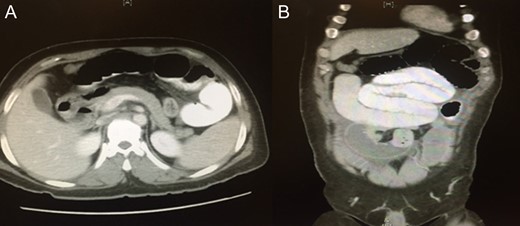
A computed tomography of the abdomen and pelvis showing small bowel obstruction at the level of the proximal ileal loops, with a transition point between dilated proximal loops and the collapsed terminal ileal loops.
The patient was initially managed conservatively, but the abdominal pain and distention did not improve. Consequently, laparoscopic-assisted abdominal exploration was performed, and the charcoal plug was removed. Intra-operatively, ~40 cm from the ileocecal junction, was a transitional zone with intramural material causing small bowel obstruction (Fig. 3). A 1.5 cm enterotomy was made, and it revealed a hard charcoal plug obstructing the small bowel (Fig. 4).

Image showing intraoperative finding of obstructing mass with transitional zone (black arrow).

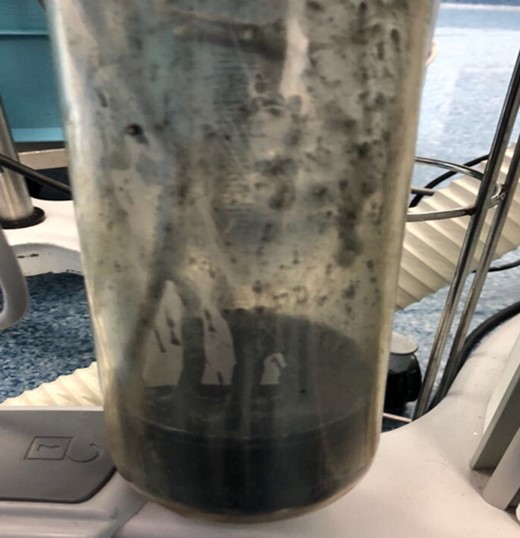
Image showing charcoal bezoars after removal from the small bowel.
The charcoal plug was removed, and the enterotomy site was closed transversely in two layers. The first layer was closed using full-thickness vicryl suture, and the second was closed using Lembert seromuscular sutures. Manual bowel decompression was performed up to the level of the duodenojejunal junction, and suctioning yielded ~1700 ml of charcoal-stained fluid (Fig. 5).
The patient’s postoperative course was uneventful. He tolerated oral intake on postoperative Day 1 and was discharged on Day 2 with close follow-up care.
DISCUSSION
Cases of bowel obstruction, although rare, have been reported in patients receiving activated charcoal. Patients at greater risk of developing an intestinal occlusion after the administration of activated charcoal appear to have a pre-existing gastrointestinal motility disorder. Other factors, including opioid or antimuscarinic drugs may increase a patient’s risk of gastrointestinal obstruction following the use of activated charcoal. The patient in our case suffered from carbamazepine overdose, which may have predisposed him to develop an intestinal obstruction after the administration of activated charcoal. In situations of overdose, carbamazepine can decrease gastrointestinal motility as a counter-regulatory measure to delay its own absorption [5]. This can trigger or cause paralytic ileus, and subsequently cause the charcoal to accumulate in the gastrointestinal tract and form bezoars.
The administration of activated charcoal can lead to constipation, and although some clinicians recommend concomitant fluid administration and gastric lavage to prevent this adverse effect, there is no consensus on this [6]. Our patient did not have concomitant fluid administration or gastric lavage. The total dose of activated charcoal that a patient receives may also play a role in intestinal obstruction, although the 150 g that our patient received was well within the recommended dosage [7]. Nevertheless, we believe the effects of carbamazepine overdose on the transit rate of the charcoal may have largely contributed to the small bowel obstruction.
Given that patients who receive activated charcoal have an increased risk of intestinal occlusion and are also prone to vomiting and subsequent aspiration, some investigators have recommended avoiding multiple-dose activated charcoal in the treatment of oral drug intoxication until there is clinical evidence of normal bowel movements in these patients [8]. Although there are concerns about the use of activated charcoal in the routine management of oral overdoses, some investigators argue that the use of activated charcoal should be encouraged in oral intoxications despite its adverse effects [9].
The clinician should suspect gastrointestinal obstruction in patients who received activated charcoal, especially when they present with charcoal-stained vomiting and abdominal pain, as was the case in our patient. Early recognition and management may help prevent necrosis of intestinal tissues and ensuing complications, such as intestinal perforation or peritonitis. In our case, conservative management was initially offered; however, this failed, prompting us to perform laparoscopic-assisted abdominal exploration to remove the charcoal plug. In isolated cases reports [10, 11], surgical removal was effective in alleviating bowel obstruction due to activated charcoal.
In conclusion, intestinal obstruction is a complication of activated charcoal administration, especially in patients who ingested medications that have antiperistaltic activity. Early identification and prompt management can help prevent fatal complications. Clinicians working in emergency departments should be informed of this rare but potential cause of intestinal obstruction to ensure better management and, consequently, improve outcomes.
Conflict of Interest statement
None declared.



