-
PDF
- Split View
-
Views
-
Cite
Cite
Hasan Dagmura, Emin Daldal, Ahmet akbaş, Fatih Daşıran, Ismail Okan, Recurrent acute pancreatitis in a patient with both gallbladder and cystic duct agenesis and polycystic liver disease, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz014, https://doi.org/10.1093/jscr/rjz014
Close - Share Icon Share
Abstract
Agenesis of the gallbladder and cystic duct is a rare congenital anomaly occurring in <0.1% of the population. However, combined gallbladder and cystic duct agenesis (CDA) with polycystic liver disease associated with recurrent acute pancreatitis (RAP) has not been reported earlier. Herein we report a case of a 36-year-old female patient who was admitted to the hospital and successfully treated for acute pancreatitis most probably caused in the background of gallbladder and CDA with polycystic liver disease. In case of non-visualization of gallbladder with the presence of biliary symptoms after repeated ultrasonographic examinations, advanced techniques like MRCP, computed tomography, EUS and even endoscopic retrograde cholangiopancreatography (ERCP) to visualize biliary anatomy must be conducted before any surgical intervention. We present a case of gallbladder and CDA causing RAP by the formation of microlithiasis treated successfully with ERCP and without any unnecessary surgery, its management and review of the literature is assessed.
INTRODUCTION
Gallbladder agenesis (GBA) is a rare condition with female gender predominance which occurs in <0.1% of the population and results from the failure of the cystic bud to develop in the fourth week of the intrauterine life [1].
Most patients with GBA and cystic duct agenesis (CDA) are asymptomatic, however those who are symptomatic present with biliary symptoms and very rarely acute pancreatitis or acute cholangitis.
Acute pancreatitis is an inflammatory condition of the pancreas characterized clinically by abdominal pain and elevated levels of pancreatic enzymes in the blood [2, 3]. The etiology of acute pancreatitis include gallstones, alcohol, hypertriglyceridemia, post-endoscopic retrograde cholangiopancreatography (ERCP), hypercalcemia, genetic mutations, drugs, infections, toxins, trauma, pancreas divisum, vascular disease, pregnancy, etc. While the most common etiologic reason is biliary origin, alcohol being the second most common cause, the rare causes of acute pancreatitis are difficult to identify and requires meticulous research. Therefore, the case reports of rare cases of acute pancreatitis carry paramount importance to spread the information.
Here we present a case of young female patient diagnosed with RAP that we assumed to be due to the agenesis of both gallbladder and cystic duct with the background of polycystic liver disease after thorough diagnostic work-up.
CASE REPORT
We present a case of a 36-year-old female patient which was admitted to our hospital with the complaints of severe epigastric pain. The pain radiated to the back and associated with vomiting, nausea, chills and loss of appetite. The patient’s medical history revealed three cesarean section, no oral contraceptive pills, no known drug allergies, no tobacco, no alcohol or illicit drug use. The patient was previously diagnosed of relatively mild two episodes of acute pancreatitis. The last one occurred 2 years ago during its last gestation trimester when she was hospitalized for 4 days and had symptomatic medical treatment. The abdominal ultrasonography performed at that time revealed a contracted gallbladder. Then, the patient was lost to follow-up.
On admission, the patient was subfebrile with denoted vital signs here: Pulse rate of 98/min, blood pressure of 100/70 mmHg and respiratory rate of 24/min. The examination of abdomen showed the presence of Pfannential incision scar and it was normal except mild distention with epigastric tenderness. Biochemical studies revealed leukocytosis (WBC: 16 s000 μl/dl, N: 4.000–10.000), elevated CRP (42, N: 0–5), elevated amylase (830, N: 25–125 U/l) and lipase (642, N: 0–140 U/l) and increased liver function tests (data not shown). Lipid profile, calcium and PTH levels were all within normal range.
The inpatient medical treatment with IV fluids, nothing per mouth and pain management was initiated. The abdominal ultrasonography showed gas distention and no visualization of the gallbladder.
The patient’s symptoms markedly resolved in 3 days after admission; she was able to tolerate oral diet and was discharged with nearly normal biochemical levels. Repeated hepatobiliary ultrasonography showed no gallbladder with minimal common bile duct dilatation. Subsequent abdominal computed tomography (CT) and MRCP (Fig. 1) confirmed the diagnosis of congenital absence of gallbladder and cystic duct with multiple hepatic cysts.
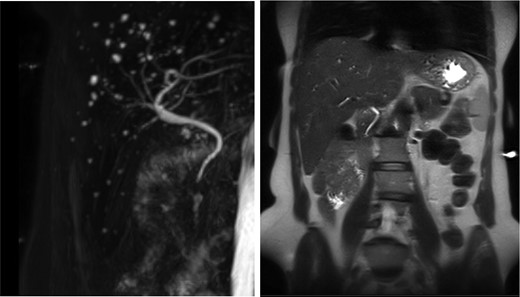
Absence of the gallbladder and the cystic canal with the presence of multiple liver cysts.
During a follow-up period of 20 months, the patient experienced three biliary colicky-like attacks complicated in one with acute pancreatitis which resolved with medical treatment and diet.
Symptomatic treatment with spasmolytics and ursodeoxycholic acid preparate was prescribed for 6 months. During this period the patient suffered another attack of pancreatitis which resolved after hospitalization again.
The patient was convinced to undertake ERCP for diagnostic and probably therapeutic purposes. During ERCP, sphincterotomy was performed and microlithiasis was detected and bile duct was cleared. Bile culture was negative and microscopic analysis of the bile showed microlithiasis due to cholesterol crystals precipitation. Follow-up for 4 years was uneventful.
DISCUSSION
GBA is a rare congenital anomaly of the biliary system which was originally reported by Lemary in 1701 [4]. This condition results from failure of development or canalization of the cystic bud in the fourth week of intrauterine life and it is often associated with other anomalies namely genitourinary tract, gastrointestinal and cardiovascular malformations.
The absence of gallbladder within the normal anatomic location does not necessarily implicate the diagnosis of GBA but it might be due to an ectopic location anywhere in the right upper quadrant mainly intrahepatic, between the leaves of the lesser omentum, in the retroperitoneum and the retrohepatic region, within the falciform ligament, or in the retroduodenal and retropancreatic areas [5].
The ultrasound (US) is the standard and routine initial imaging technique for the hepatobiliary diseases. However, the non-visualization of gallbladder does not simply imply a diagnosis of gallbladder agenesis, Though US examination has a high sensitivity and specificity for gallbladder pathology, the accuracy of US is not 100% due to its operator-dependency and variability of gallbladder in the host such as ectopic gallbladder, contracted gallbladder, the body habitus and bowel distention. In this context appropriate use of additional investigative modalities such as CT scan, MRCP, endoscopic US, ERCP and HIDA scan, will help to put the diagnosis preoperatively and therefore avoiding unnecessary surgery.
An observation that is worthy to mention is that while it is common for the common hepatic duct and or common bile duct to dilate after cholecystectomy with a rate of 0,04 mm year this is not the case for GBA and CDA.
GBA has been associated with a genetic predisposition [6]. Studies conducted by Yamashita et al. [7] demonstrated that Lgr4 (leucine-rich repeat-containing G protein-coupled receptor 4) gene trapped mice demonstrated only gallbladder and CDA without the involvement of adjacent structures during gestation which means that this Lgr4 is responsible for cystic duct and gallbladder genesis. The Absence of the GB may produce pancreatic changes through increased bile pressure, lack of protective mucus in the bile and biliary dyskinesia leading to the formation of intrahepatic and extrahepatic sludge and microlithiasis. The presence of more than 20 liver cysts in MRI studies indicates the presence of polycystic liver disease which may necessitate close follow-up. Isolated polycystic liver disease is a less common disorder, which is autosomal dominant and distinct from polycystic kidney disease, since it is not associated with kidney involvement or cerebral aneurysms. Two mutations have been found to cause this disorder: a mutation in the PRKCSH gene that encodes a protein called hepatocystin [8], and a mutation in the SEC63 gene that encodes for a component of the protein translocation machinery in the endoplasmic reticulum [9]. Whether the presence of GBA, CDA and polycystic liver disease in a patient is just a mere association or manifestation of a new genetic entity require further consideration and research.
Acute pancreatitis is an inflammatory process of the pancreas diagnosed with acute onset of abdominal pain and elevated pancreatic enzymes (amylase or/and lipase). It is caused by gallstones in ~45%, alcohol intake in 20–25%, post-ERCP in 5–7%, and miscellaneous in ~5% of cases [10]. After thorough investigations, up to 25% of the cases of acute pancreatitis is said to be idiopathic. The majority of acute pancreatitis (70–80%) attacks are mild and called interstitial pancreatitis, whereas the rest of the cases run a severe form known as necrotizing type and is associated with high mortality (up to 40%) and morbidity. A substantial number of patients with ‘idiopathic’ pancreatitis and unexplained biliary pain turn out to have small gallstones that have gone undetected by abdominal US or CT. The term ‘biliary microlithiasis’ was coined to describe gallstones of <2–3 mm in diameter. Microliths are predominantly composed of cholesterol. The diagnosis of microlithiasis can be suspected on bile microscopy obtained during ERCP which might show cholesterol monohydrate, calcium bilirubinate and/or calcium carbonate crystals. Microlithiasis has been recognized as a possible cause of idiopathic pancreatitis in adults.
Review of the literature showed that many cases of AGB were diagnosed intraoperatively. The patients were usually misdiagnosed ultrasonographically for contracted gallbladder and underwent cholecystectomy. During the operation, the surgeon usually is stunned by the absence of gallbladder and converts to the open surgery and proceed with extensive explorations in vain. However, our case was diagnosed in the beginning as contracted gallbladder, the preoperative search with CT and MRCP revealed the misdiagnosis with confirmation of AGB. The high index of suspicion saved the patient from unnecessary surgery.
We hypothesized in our patient that the underlying etiology of recurrent acute pancreatitis attacks was due to the microlithiasis formed in common bile duct because of congenital absence of the gallbladder. Agenesis of gallbladder might have caused abnormal changes in the bile composition with the absence of cytoprotective effect of mucin. Our patient had relatively short and mild recurrent acute pancreatitis attacks which resolved with short hospitalization and conservative treatment. ERCP is an appropriate modality to treat microlithiasis in such rare cases. In our case, the repeated attacks of acute pancreatitis led us to consider ERCP both for diagnosis and treatment of putative microlithiasis.
CONCLUSION
Agenesis of gallbladder and cystic duct is a very rare condition which might be the cause of recurrent acute pancreatitis. The preoperative diagnosis saves the patients from unnecessary surgery. Therefore, high suspicion index could help the physician to establish the correct diagnosis with proper diagnostic procedures like CT, MRCP, EUS and ERCP. ERCP can be used both for the diagnosis and the treatment of microlithiasis which might be the underlying pathology for the recurrent attacks of pancreatitis.
CONFLICT OF INTEREST STATEMENT
None declared.



