-
PDF
- Split View
-
Views
-
Cite
Cite
Richesh Guragain, Alawadi Zeinab, Monica Cheng, Prava Karki, John B Holcomb, Primary midgut volvulus in a patient with Marfan syndrome, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz031, https://doi.org/10.1093/jscr/rjz031
Close - Share Icon Share
Abstract
Marfan syndrome is a mutation in the fibrillin-1 gene resulting in a connective tissue disorder primarily affecting musculoskeletal, cardiovascular and ocular systems. However, patients with Marfan’s rarely manifest gastrointestinal symptoms. Midgut volvulus is abnormal twisting of small bowel around its mesentery that can result in compromising blood flow to the bowel causing intestinal ischemia and obstruction. Primary midgut volvulus is a term used when there is no underlying cause for the volvulus. This case describes an 80-year-old female with Marfan syndrome presenting with primary midgut volvulus, which preoperatively was suspected based on imaging, and later confirmed upon operative exploration. The small bowel mesentery was long with a narrow base twisted around its mesentery 360°. The long narrow base and floppy mesentery likely contributed to hypermobility leading to volvulus and small bowel obstruction. To our knowledge, this is the first reported case of primary midgut volvulus associated with Marfan’s syndrome.
INTRODUCTION
Marfan syndrome can encompass an array of anatomical abnormalities most often involving soft tissue dysmorphia and cardiovascular pathology, but rarely includes gastrointestinal pathology [1–3]. Midgut volvulus is torsion of small bowel along the axis of the superior mesenteric artery in a compromising manner that endangers the viability and future function of the twisted segment if not intervened immediately [1–3]. While secondary small bowel volvulus is most commonly due to anatomical abnormalities like intestinal malrotation and diverticulum [1]; primary midgut volvulus is unique in location and has no known underlying etiology. Even though the etiology and mechanism of mesenteric rotation in primary midgut volvulus is not fully understood, it is widely agreed that unusually hypermobile bowel rotates around mesentery in absence of adhesions or congenital abnormalities [4]. The exact incidence and prevalence of gastrointestinal complications of Marfan syndrome is not known [3]. Regardless of etiology, the clinical presentation of midgut volvulus is the same. It commonly manifests with pain, vomiting and nausea [2]. The clinical presentation, evaluation, workup and operative management of our patient with midgut volvulus in a patient with long standing diagnosis of Marfan syndrome diagnosis is described below.
CASE REPORT
This case report presents an 80-year-old female with past medical history of Marfan syndrome with extensive cardiovascular manifestations including coarctation of the aorta, mechanical aortic valve and mitral valve replacement, heart failure with reduced ejection fraction (25–30%), and atrial fibrillation. The patient was admitted to the emergency general surgical service for complaints of acute onset colicky periumbilical abdominal pain, progressive abdominal distension, nausea and vomiting for 2 days. Emesis was described as non-bloody and non-bilious. Other pertinent history included one bowel movement 12 h prior to admission, which was non-bloody and inability to pass flatus for more than 24 h. No previous episode of abdominal pain of similar nature were elicitated. Physical examination was significant for mild abdominal distension and generalized tenderness to palpation in all quadrants without signs of peritonitis. Patient was afebrile and hemodynamically stable. Significant laboratory findings were INR of 2.20 (on warfarin for valve replacement), hyponatremia of 125, acute kidney injury with creatinine of 1.56. computed tomography (CT) of the abdomen/pelvis was significant for high-grade small bowel obstruction with a swirling of the superior mesenteric artery (SMA) and superior mesenteric vein (SMV) suggesting rotation of intestinal mesentery (Fig. 1) [5]. The SMV was located to the right of SMA, a reliable finding against intestinal malrotation [5] (Fig. 2). Further, there was no radiologic evidence of malrotation like transposition of SMA and SMV, the horizontal part of the duodenum not reaching medioventral line, and malposition of ileocecal junction [5]. The INR was not reversed with FFP and Vitamin K due to concern for stroke. Emergent exploratory laparotomy within 6 h of admission was performed which was significant for midgut volvulus with the small bowel rotating around the base of mesentery a complete 360°. There were no signs of ischemia, and hence manual untwisting of the bowel was performed [2, 5]. The cecum was noted to be on the right lower quadrant and ligament of Treitz was on the left upper quadrant. The small bowel mesentery was noted to appear long with narrow base and floppy likely contributing to hypermobility of the small bowel. The patients postoperative course was uneventful, and she was discharged to skilled nursing facility for further rehabilitation.
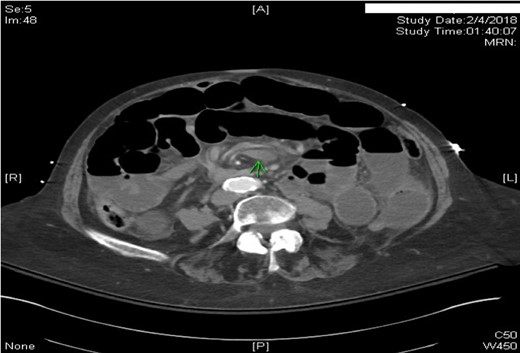
Axial CT scan of Abdomen with IV contrast: Swirling of the superior mesenteric artery and superior mesenteric vein. Proximal and mid small bowel dilatation with differential air–fluid level.
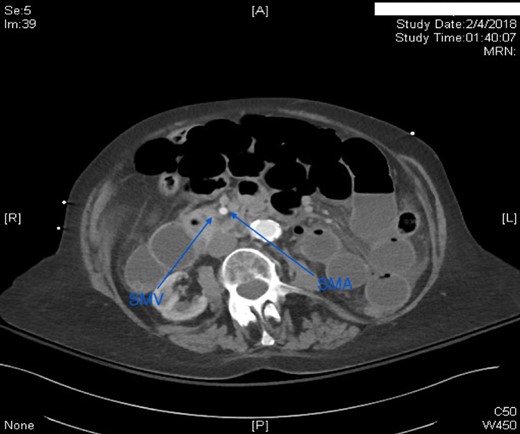
Axial CT scan of abdomen with IV contrast. SMV was located to the right of SMA.
DISCUSSION
Marfan syndrome is an autosomal dominant inherited connective tissue disorder resulting from a genetic mutation in the fibrillin-coding gene, FBN1 [6]. Fibrillin is a glycoprotein critical for the appropriate production of elastic microfibrils, which form the scaffold to build stronger elastic fibers [6]. Microfibrils store and manage the availability of TGF-β to maintain proliferation, differentiation, motility and apoptosis of other cells [6]. The mutation in the fibrillin gene results in weakened connective tissues throughout the body, leading to varying multisystem dysfunction for those with Marfan syndrome [2, 6]. While Marfan syndrome causes abnormal findings manifest in many systems, gastrointestinal presentations are infrequent and there are only a few cases reported of differing diagnoses, most of the cases presenting with abnormal anatomy of various segments of the gastrointestinal system such as diverticulosis coli, hernias, diveriticula, atresias, malrotations and sigmoid volvulus [1, 3, 7–9].
Our patient’s history was significant for extensive cardiovascular involvement including mechanical aortic valve and mitral valve replacement, but no previous gastrointestinal involvement was noted. Upon review of the literature, there have been a few reported cases of small bowel diverticulosis, especially of the jejunal area, and a few reported cases of sigmoid volvulus in conjunction with a diagnosis of Marfan syndrome [3, 7, 8]. Jejunal volvulus reported was in a patient with no known history of Marfan syndrome and was likely due to massive jejunal diverticula from unknown cause ranging from 3.5 to 8 cm [7]. There are no reported cases of primary midgut volvulus in conjunction with a diagnosis of Marfan syndrome. Primary midgut volvulus is more commonly seen in a population that ranges from infants to young adults whereas midgut volvulus with a secondary cause is more likely to be seen in older adults [2]. Furthermore, primary midgut volvulus is more prevalent in lower socioeconomic status, regions like Middle east, Asia and Central Africa, associated with consumption of bulky indigestible meals after fasting, and hypermobility of the mesentery [4]. Our patient finding of long and floppy mesentery is likely contributory to her presentation of primary midgut volvulus resulting in small bowel obstruction.
Intestinal malrotation is a very common cause of midgut volvulus in the pediatric population. Malrotation may result from predisposing genetic mutations and are often found in conjunction with other congenital malformations [1, 2, 5, 10]. Since malrotations are often obvious in infants and children, adults with intestinal malrotation are often found incidentally during non-related abdominal surgeries [5, 10]. There was no evidence of intestinal malrotation in our patient.
CONCLUSION
Gastrointestinal pathology is not commonly found in patients with Marfan syndrome compared to higher occurrences of cardiovascular, ocular and soft tissue pathology. While cases of volvulus have been reported in those with Marfan syndrome, these cases are rare and reported in the sigmoid location and often secondary to adhesions. The very few cases involving midgut pathology in patients with Marfan syndrome were cited to be diverticulosis and without volvulus. To our knowledge this is the first case reported of Marfan syndrome and primary midgut volvulus and through this case report information is provided to guide further study and care of gastrointestinal manifestations in those with a concurrent diagnosis of Marfan syndrome.
Acknowledgements
Dr Holcomb is the Chief Medical Officer of Prytime Medical, the Founder and on the Board of Directors of Decisio Health, and a consultant to Arsenal Medical and Terumo.
Conflict of Interest statement
None.
REFERENCES
- gastrointestinal tract vascular insufficiency
- marfan syndrome
- small bowel obstruction
- vascular flow
- mutation
- connective tissue diseases
- cardiovascular system
- genes
- intestine, small
- intestines
- mesentery
- signs and symptoms, digestive
- diagnostic imaging
- intestinal volvulus
- malrotation, congenital
- hypermobility
- fibrillin-1



