-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel R Principe, Jonathan Rubin, Andreea Raicu, Colleen Hagen, Massive adult cystic lymphangioma of the breast, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz027, https://doi.org/10.1093/jscr/rjz027
Close - Share Icon Share
Abstract
Adult cystic lymphangiomas are exceedingly rare tumors resulting from malformation of the lymphatic vessels. Like their pediatric counterparts, these lesions almost exclusively involve the head and neck. However, adult cystic lymphangiomas have been reported in several organs. Those involving the breast are exceptionally rare, with only a few reported instances. Here, we present the case of a 27-year-old woman who attended a surgical breast clinic with a 2-year history of a large, disfiguring left breast mass. Pathology was consistent with adult cystic lymphangioma of the breast. Measuring 21.0 × 20.0 × 6.0 cm3, this represents the second largest of its kind and the largest reported case in an African American patient.
INTRODUCTION
Cystic lymphangiomas (hygromas) comprise a cluster of rare tumors commonly found in children. In these cases, regional lymph drainage is obstructed due to a congenital malformation of lymphatic vessels, resulting in lymph node degeneration, inflammation and fibrosis of existing lymph channels [1]. Lymphangiomas are almost universally benign tumors, though rare instances of malignant transformation have been reported [2, 3]. The overwhelming majority of cystic lymphangiomas are found in the head, neck (most often the left posterior triangle) or the axilla. Hence, while benign, these tumors can be disfiguring and given the most frequent areas of presentation, can affect breathing/swallowing. Very rarely, cystic lymphangiomas can develop outside of the neck or axilla, predominantly in the mediastinum, retro-peritoneum, pelvis or groin [4].
Half of cystic lymphangiomas are present at birth, and 90% are diagnosed by age 2 [3, 5]. Though generally a pediatric issue, cystic lymphangiomas can present in adults. Adult cystic lymphangiomas are also most prevalent in the neck, but have been observed in several different organ systems [4]. Cystic lymphangiomas of the breast have also been reported, though these are exceptionally rare. Here, we describe the diagnosis and management of one of the largest breast lymphangiomas ever reported, and the largest reported case in an adult African American patient.
CASE REPORT
A 27-year-old African American female who presented to an outpatient surgical breast clinic complaining of a large left breast mass for 2 years. Her previous medical history was unremarkable, and she had no family history of breast or ovarian cancer. Although the mass was clearly visible and distorted her breast, she was otherwise asymptomatic denying pain, skin discoloration or nipple discharge. Two years before presenting to our clinic, the patient had been seen for this mass at our institution. At this time, the mass measured ~18 cm in length, and was located in 2:00 position 23 cm from the nipple. A mammogram was performed, and the lesion categorized as Breast Imaging-Reporting and Data System (BI-RADS 2A). The patient also underwent an ultrasound-guided fine needle aspiration (FNA), after which the lesion was drained, yielding over one liter of sanguineous, non-purulent, straw colored fluid. FNA samples were sent to pathology, and cytology report indicated that the mass was likely a lymphangioma given the high presence of lymphocytes, scant histiocytes and isolated tingle-body macrophages. The patient was offered surgery at this time, but was lost to follow up until returning to our clinic 2 years later.
In this most recent visit, her physical examination was normal apart from the left breast mass, and the patient showed no obvious signs of distress. Breast exam was consistent with her previous diagnosis, showing a roughly 20 × 10 cm2 lobulated, fluid-filled, left breast mass. Given the large size, imaging was recommended to the patient in order to better evaluate the extent of the mass. Diagnostic mammogram revealed a 23.6 × 15.7 × 15.1 cm3 lobulated mass in the lateral left breast, again categorized as BI-RADS 2A (Fig. 1A). This was confirmed via ultrasound and computed tomography (CT) (Fig. 1B and C). Given her history and the results of cytopathology, we concluded that this was most likely a persistent cystic lymphangioma of the breast, but repeated pathologic analysis to exclude the possibility of malignant transformation or breast cancer.
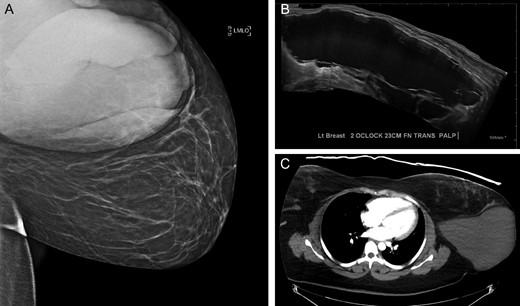
Results of pre-operative (A) mammography (B) ultrasound and (C) computed tomography (CT).
The patient was brought back to the outpatient breast center to discuss imaging results and surgical options. She elected to proceed with surgical excision of the mass given the size and its distorting nature (Fig. 2A). Due to insurance issues, the patient was unable to have immediate reconstruction with a plastic surgeon. One week later, the patient was scheduled for excision of the left breast mass (Fig. 2B and C). She tolerated the procedure well without any complications, and she was comfortable going home the same day on minimal analgesia. The final pathology report was consistent with lymphangioma (Fig. 3), showing a 21.0 × 20.0 × 6.0 cm3 mass that contained nearly 800 mL of serosanguinous fluid. The cyst wall varied in thickness from 0.1 to 0.2 cm. Post-operatively, the patient did well with no wound complications or complaints. She was referred to plastic surgery for delayed reconstruction at an outside institution.

(A) Pre-operative photograph of the left breast mass. (B) Intraoperative resection of mass. (C) Gross pathology of resected mass.
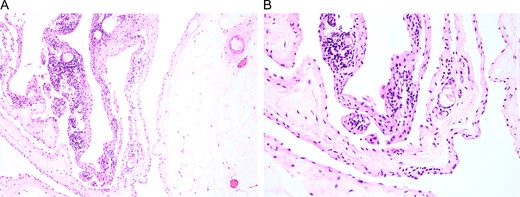
Surgical specimens were collected and stained with H&E. Representative images are shown at (A) low and (B) high magnification, which affirmed the diagnosis of cystic lymphangioma.
DISCUSSION
Adult cystic lymphangiomas are exceedingly rare, particularly those involving the breast. Of the known cases, most are located in the upper, outer quadrant of the breast, as this area contains ~75% of the lymphatic drainage toward the axilla [6]. The precise etiology of adult lymphangiomas is unclear. Like those found in children, they are believed to stem from malformations resulting from either hyperproliferation of lymphatic vessels, weakness in the lymphatic walls or other obstruction of the lymphatic drainage [7]. Malignant transformation of cystic lymphangioma of the breast has not been reported and these tumors are generally painless. Hence, most are treated cosmetically. However, with any breast mass malignancy should be suspect until confirmed otherwise.
Hence, with any new breast mass regardless of history, diagnosis should be made quickly in order to determine the appropriate treatment course. This can be aided through the use of multiple radiographic modalities including mammogram, ultrasound, CT and magnetic resonance imaging (MRI). Of these options, MRI has been suggested to be the most informative, as lymphangiomas generally show low intensity of T1 and high intensity on T2 images. Additionally, there is enhancement of the septa, with tumors often appearing multiseptated [8].
FNA can be also be used to aid pre-op diagnosis, however, the gold standard for diagnosis is made through excisional biopsy. Surgical excision is in fact primary treatment modality for these lesions, providing the lowest rate of recurrence [8]. However, for patients in whom surgery is contraindicated, guided percutaneous sclerosis can be performed [9]. Ultimately, both approaches offer a significant benefit and should be considered based on patient preference and practitioner discretion.
CONFLICT OF INTEREST
The authors have no conflicts to disclose.
FUNDING
D.R. Principe is supported by the National Cancer Institute of the National Institutes of Health under Award Number F30CA236031.



