-
PDF
- Split View
-
Views
-
Cite
Cite
Vaanathi Paulvannan, Seshukumar Bylapudi, Mithun Kumar Ramesh Kumar, Mahesh Nachimuthu, Paulvannan Subramanian, Perforation of Heterotopic Gastric Mucosa in ileal duplication in an adult: A case report, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz025, https://doi.org/10.1093/jscr/rjz025
Close - Share Icon Share
Abstract
Bowel duplication with heterotopic gastric mucosa (HGM) is a known but uncommon pathology. It usually presents with intussusception or melena in the early years of life. We present a case of ileal duplication with HGM with a rare presentation of bowel perforation and peritonitis in an adult male.
INTRODUCTION
Duplication of the gastrointestinal tract is a rare pathology. It is estimated to occur in one in every 4500 births [1]. Most cases of duplicated bowel present during childhood [2]. These duplicated bowel loops may contain Heterotopic Gastric Mucosa (HGM). The presentations of HGM include obstruction, intussusception and mucosal ulceration with bleeding. Here, we discuss a rare case of peritonitis due to perforation in an ileal duplication presenting in an adult male.
CASE REPORT
A 27-year-old male presented to a local hospital with sudden onset of severe abdominal pain. Examination revealed features of peritonitis. An emergency laparotomy showed purulent peritonitis but the site of perforation could not be identified. Peritoneal washout was done, drains were kept and the abdomen was closed. During the post-operative period, the patient’s condition worsened with high spikes of fever and oliguria. A contrast enhanced CT of the abdomen showed only dilated bowel loops. The patient was referred for further management to a tertiary referral center.
On arrival, he had features of septic shock and signs of peritonitis. The abdominal drains showed coffee colored fluid mixed with blood clots. Blood investigations revealed leukocytosis, normal lipase and elevated serum creatinine. Blood gas analysis showed compensated metabolic acidosis. The patient was admitted to the ICU and resuscitated with fluids. Empirical broad spectrum antibiotics (Meropenem and Teicoplanin) and inotropes were started along with Non Invasive Ventilatory support.
Once the patient’s condition had improved, he was taken for an emergency re-look laparotomy. Intra-operatively, there was a blind loop of ~90 cm arising from the terminal ileum, which was identified to be a duplicated bowel loop. This loop showed multiple perforations (Figs 1 and 2), all of which were draining coffee colored fluid suggestive of acid hematin. However, there were no small bowel contents in the peritoneal cavity which rose suspicions of HGM in the duplicated bowel loop. The duplicated bowel with its junction with the normal terminal ileum was resected and a side to side (functional end to end) small bowel anastomosis was done. Post operatively the patient was monitored in the ICU with inotropes and ventilatory support. He showed a gradual improvement and was subsequently discharged. The histopathology of the resected specimen showed extensive HGM with multiple ulcerations and perforations.
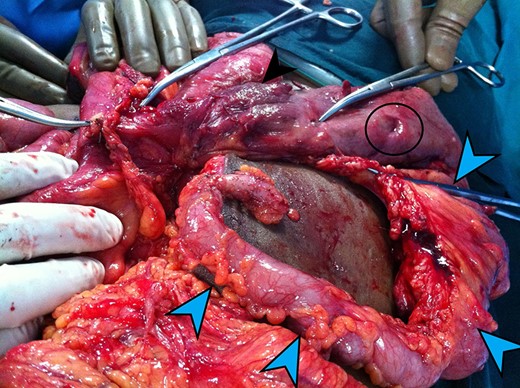
The Blue arrows outline the duplicated bowel loop. Black arrow shows the normal bowel. The black circle shows one of the perforations in the duplicated loop.
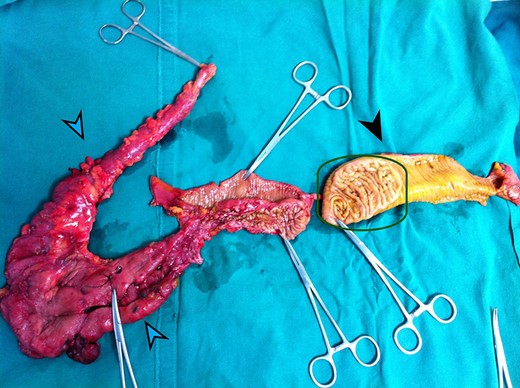
The Blue arrows outline the duplicated bowel loop. The Black arrow shows the normal bowel. The Green square outlines a thickened patch of mucosa at the site of communication of duplicated bowel with the ileum.
DISCUSSION
The etiology of GI tract duplications remains unknown. Several theories such as defective recanalization, partial twinning, split notochord theory and persistence of fetal gut diverticula remain at the forefront. Among the instances of GI tract duplications, it is most commonly reported in the jejunum and ileum [3]. The two types of duplications are cystic and tubular. Small cystic duplications can act as lead points for intussusception or can result in volvulus. Long tubular duplications can communicate proximally or distally [4]. Proximal communications drain poorly, and retention of intestinal contents can cause obstruction and act as a blind loop causing small intestinal bacterial overgrowth. Distal communications, as seen in our patient, are rarely symptomatic unless there is presence of HGM. Bowel duplication can also present in the form of an echogenic duplication cyst [3]. In some cases, bowel duplications remain to be an incidental finding. However, when they contain HGM, they predominantly become symptomatic.
Ectopic gastric mucosa was first described by Schmidt in 1805 [5]. It is classified into heterotopic (congenital) and metaplastic (acquired). Correspondingly, two pathological types have been reported: the more common type, which is associated with the congenital type shows gastric gland and foveolar epithelium. The other type which is believed to occur in the metaplastic type shows only foveolar epithelium [6]. In our patient, the presence of coffee brown fluid was suggestive of acid hematin. It is known that acid hematin is the acid salt of HCl acting on hemoglobin [7], which implies the presence of gastric glands in the loop. Correspondingly, the histopathology showed gastric glands which led to the development of several ulcers and their perforation.
Most cases of symptomatic HGM occur in children in the first year of life [2]. Our patient presented with the first onset of symptoms at 27 years of age. The occurrence of HGM in bowel duplications occurs in only 17–36% of cases [8]. Most cases of duplication present with intussusception, obstruction and melena [4]. Presentations like intestinal perforation with peritonitis [4] or carcinoma [9] is relatively rare. A few cases have also been reported of the patients developing a chronic illness like failure to thrive [10].
In less acute presentations, HGM can be diagnosed using various modalities. 99mTc-Pertechnetate scan is very effective. Abdominal ultrasound can be used to diagnose only the spherical type of duplication. In slightly more complicated cases, CT scans have also been known to play a role [3]. However, it remains that in acute presentations, such as in our patient, the only option is immediate surgery. It is clear that the only treatment option for a symptomatic and especially a perforated bowel segment, is resection and anastomosis as early as possible [2].
Although a rare presentation, duplicated bowel may also become symptomatic in adults. A Long duplicated bowel loop may mimic the normal small bowel, and may even be overlooked in a laparotomy, as in our patient’s first surgery. Absence of bowel contents with the presence of acid hematin and bowel perforation should raise suspicions of HGM in a duplicated bowel loop. If the perforation in our patient had been diagnosed during the first surgery, all the further complications could have been avoided. A thorough examination of the bowel loops during the laparotomy in these circumstances would help to identify the rare abnormal loop and a definitive treatment in the form of resection of the duplicated bowel with its attachment with the normal bowel can be undertaken.
CONFLICT OF INTEREST STATEMENT
None declared.



