-
PDF
- Split View
-
Views
-
Cite
Cite
Ilias Vagios, Aphrodite Nonni, Aliki Liakea, Anastasia Constantinidou, Michael Kontos, Intraductal papilloma of the male breast: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz023, https://doi.org/10.1093/jscr/rjz023
Close - Share Icon Share
Abstract
Intraductal papilloma is a benign neoplasm rarely found in the male breast. In this report, we present the case of a 55-year-old Caucasian man who presented with spontaneous bloody nipple discharge of the right breast. Ultrasonic and mammographic investigations revealed a sub-centimetre solid mass within a dilated duct. He underwent a total duct excision. Histopathologic examination confirmed a benign intraductal papilloma with no evidence of atypia or malignancy. A systematic review of the literature revealed six published cases of intraductal papillomas in men. Clinical presentation is the same as in women with single duct blood stained discharge being the most common presenting symptom. Surgical excision offers both histologic confirmation and definitive treatment. There is one case where the lump was not removed and progressed to malignancy years later. Male intraductal papillomas may be associated to medical treatments with hormonal activity given for other reasons or endocrine abnormalities.
INTRODUCTION
Intraductal papilloma (IP) is a prolifrative lesion of the mammary duct. It is usually entirely benign but can occasionally host atypical or even malignant cells. The benign IP consists of an epithelium containing both luminal and myoepithelial cells and abundant stroma, forming a few broad fronds [1]. The variants of IP include central papilloma (large-duct papilloma) and peripheral papilloma (small-duct papilloma) [2]. IPs of the male breast are a very rare condition in breast pathology, with very few reported cases in the literature. We report the case of a 55-year-old man with a tumour proving to be a solitary intraductal papilloma and we present the results of a literature review of this condition.
CASE REPORT
A 55-year-old Caucasian man, with unremarkable medical and breast history presented at our outpatient clinic complaining of bloody discharge from his right nipple of 1 month duration. Physical examination confirmed a single-duct bloody discharge, however no mass was palpated (Fig. 1). Mammography showed the patterns of mild gynaecomastia and a round well-circumscribed mass of 1 cm in diameter just inferior to the nipple.

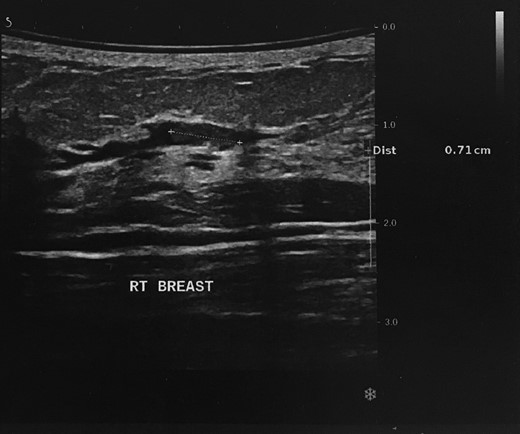
Ultrasound revealed that the well-circumscribed mass was a simple cyst; however, there was an additional hypoechoic solid mass of 0.7 cm in maximum diameter within a single dilated duct, compatible with an intraductal papilloma (Fig. 2). Axillary lymph nodes were benign. The mass was graded as 4 on the BIRADS (Breast Imaging Reporting and Data System) scale.
Cytological examination of the nipple discharge was negative for malignancy.
The patient underwent total duct excision on the right, through a circumareolar incision and the specimen was sent for pathologic review. There were no postoperative complications, a good cosmetic result was achieved and the patient was discharged on the same day.
The histologic examination revealed an intraductal papilloma of 9 mm in maximum diameter with no evidence of atypia or malignancy (Figs 3,4 and 5).
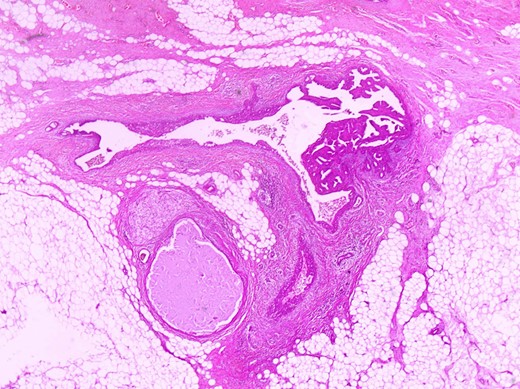
Partially dilated duct with papillary projections within its lumen (in the right side of it) (H+Ex400).
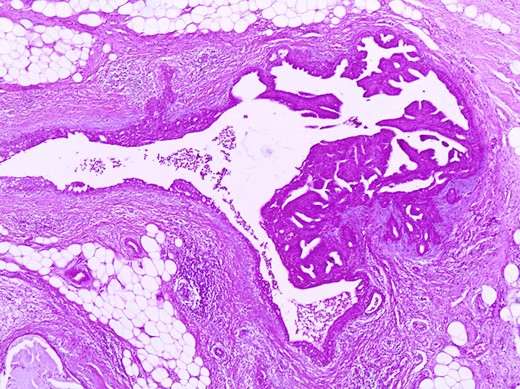
The same duct with the papillary projections. The wall is fibrotic and there are also foci of usual type of epithelial hyperplasia (H+E×100).
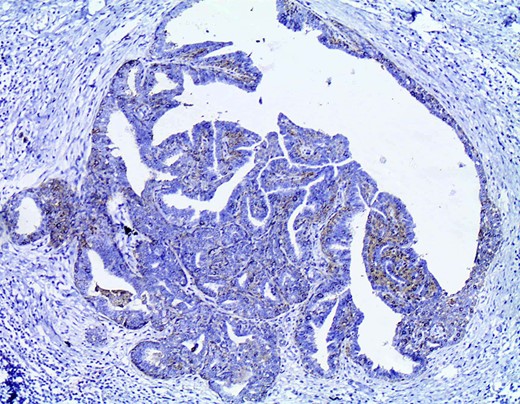
Immunohistochemistry with CK14 demonstrates the myoepithelial cells in the papillary structures (CK14×200).
DISCUSSION
IPs of the male breast are rare as opposed to papillomas in women. They account for 40–70% of pathological nipple discharge in women. About 5–10% of patients with blood-stained discharge will be found to have an underlying malignancy. Single duct, bloody discharge, discharge associated with a mass or discharge in patients over 50-years old are risk factors for cancer [3]. The diagnostic approach of intraductal papillary lesions includes physical examination, mammography, ultrasonography, MRI and more rarely mammary ductoscopy or ductography; cytological examination of the discharge can also be used [4].
The differential diagnosis between benign IP and a carcinoma containing atypia or even malignancy is not feasible through imaging alone, thus surgical excision and histological confirmation is required [3]. Clinically, papillomas produce spontaneous serous or bloody nipple discharge, occasionally associated with a palpable mass under or around the nipple-areola complex.
In the present study, the case of a 52-year-old man with an intraductal papilloma of the right breast, causing single duct bloody discharge is presented. Clinical examination was highly suspicious of an intraductal papilloma despite its rarity in men. The imaging results were reported as BIRAS4 and compatible with the clinical suspicion. The diagnosis was confirmed through histological analysis which revealed an intraductal papilloma with no evidence of atypia or malignancy.
A systematic search in PubMed (English language) revealed only six cases of IPs in men. Patient and tumour characteristics, as well as treatment were identified and are presented in Table 1.
| Report . | Age . | Nipple discharge . | Palpation . | Side/tenderness or pain . | Histological diagnosis and treatment . | Histopathology . | Comorbidities and relevant medical history . |
|---|---|---|---|---|---|---|---|
| Gaurav et al. [5] | 52 | Bloody | Swelling of the breast three years after the biopsy | RB/painless | Core biopsy for initial diagnosis—right simple mastectomy for the treatment of the malignant tumour | Intraductal papilloma progressing to invasive ductal carcinoma three years later | Hypertension |
| Sara et al. [7] | 71 | Bloody | Palpable | LB/- | Excision | Intraductal papilloma, 100 mm | Psychiatric disorders- phenothiazines |
| Tsilimigras et al. [9] | 11 | Bloody | Palpable | RB/- | Excision | Intraductal papilloma, 8 mm | Malignant brain tumour, kryptorchidism |
| De Vries et al. [8] | 29 | - | Palpable | LB/tender | Excision | Intraductal papilloma, 10 mm | Use of steroids |
| Durkin et al. [6] | 14 | - | Palpable | LB/- | Excision | Intraductal papilloma, 40 mm | Family history of infiltrating breast cancer (mother, aunt) |
| Szabo et al. [10] | 42 | Bloody | Non palpable | LB/- | Sector resection | Intraductal papilloma | Bilateral gynaecomastia |
| Present study (2018) | 52 | Bloody | Non palpable | RB/painless | Total duct excision | Intraductal papilloma, 9 mm | Unilateral gynaecomastia |
| Report . | Age . | Nipple discharge . | Palpation . | Side/tenderness or pain . | Histological diagnosis and treatment . | Histopathology . | Comorbidities and relevant medical history . |
|---|---|---|---|---|---|---|---|
| Gaurav et al. [5] | 52 | Bloody | Swelling of the breast three years after the biopsy | RB/painless | Core biopsy for initial diagnosis—right simple mastectomy for the treatment of the malignant tumour | Intraductal papilloma progressing to invasive ductal carcinoma three years later | Hypertension |
| Sara et al. [7] | 71 | Bloody | Palpable | LB/- | Excision | Intraductal papilloma, 100 mm | Psychiatric disorders- phenothiazines |
| Tsilimigras et al. [9] | 11 | Bloody | Palpable | RB/- | Excision | Intraductal papilloma, 8 mm | Malignant brain tumour, kryptorchidism |
| De Vries et al. [8] | 29 | - | Palpable | LB/tender | Excision | Intraductal papilloma, 10 mm | Use of steroids |
| Durkin et al. [6] | 14 | - | Palpable | LB/- | Excision | Intraductal papilloma, 40 mm | Family history of infiltrating breast cancer (mother, aunt) |
| Szabo et al. [10] | 42 | Bloody | Non palpable | LB/- | Sector resection | Intraductal papilloma | Bilateral gynaecomastia |
| Present study (2018) | 52 | Bloody | Non palpable | RB/painless | Total duct excision | Intraductal papilloma, 9 mm | Unilateral gynaecomastia |
-: unknown.
RB/LB: right and left breast
| Report . | Age . | Nipple discharge . | Palpation . | Side/tenderness or pain . | Histological diagnosis and treatment . | Histopathology . | Comorbidities and relevant medical history . |
|---|---|---|---|---|---|---|---|
| Gaurav et al. [5] | 52 | Bloody | Swelling of the breast three years after the biopsy | RB/painless | Core biopsy for initial diagnosis—right simple mastectomy for the treatment of the malignant tumour | Intraductal papilloma progressing to invasive ductal carcinoma three years later | Hypertension |
| Sara et al. [7] | 71 | Bloody | Palpable | LB/- | Excision | Intraductal papilloma, 100 mm | Psychiatric disorders- phenothiazines |
| Tsilimigras et al. [9] | 11 | Bloody | Palpable | RB/- | Excision | Intraductal papilloma, 8 mm | Malignant brain tumour, kryptorchidism |
| De Vries et al. [8] | 29 | - | Palpable | LB/tender | Excision | Intraductal papilloma, 10 mm | Use of steroids |
| Durkin et al. [6] | 14 | - | Palpable | LB/- | Excision | Intraductal papilloma, 40 mm | Family history of infiltrating breast cancer (mother, aunt) |
| Szabo et al. [10] | 42 | Bloody | Non palpable | LB/- | Sector resection | Intraductal papilloma | Bilateral gynaecomastia |
| Present study (2018) | 52 | Bloody | Non palpable | RB/painless | Total duct excision | Intraductal papilloma, 9 mm | Unilateral gynaecomastia |
| Report . | Age . | Nipple discharge . | Palpation . | Side/tenderness or pain . | Histological diagnosis and treatment . | Histopathology . | Comorbidities and relevant medical history . |
|---|---|---|---|---|---|---|---|
| Gaurav et al. [5] | 52 | Bloody | Swelling of the breast three years after the biopsy | RB/painless | Core biopsy for initial diagnosis—right simple mastectomy for the treatment of the malignant tumour | Intraductal papilloma progressing to invasive ductal carcinoma three years later | Hypertension |
| Sara et al. [7] | 71 | Bloody | Palpable | LB/- | Excision | Intraductal papilloma, 100 mm | Psychiatric disorders- phenothiazines |
| Tsilimigras et al. [9] | 11 | Bloody | Palpable | RB/- | Excision | Intraductal papilloma, 8 mm | Malignant brain tumour, kryptorchidism |
| De Vries et al. [8] | 29 | - | Palpable | LB/tender | Excision | Intraductal papilloma, 10 mm | Use of steroids |
| Durkin et al. [6] | 14 | - | Palpable | LB/- | Excision | Intraductal papilloma, 40 mm | Family history of infiltrating breast cancer (mother, aunt) |
| Szabo et al. [10] | 42 | Bloody | Non palpable | LB/- | Sector resection | Intraductal papilloma | Bilateral gynaecomastia |
| Present study (2018) | 52 | Bloody | Non palpable | RB/painless | Total duct excision | Intraductal papilloma, 9 mm | Unilateral gynaecomastia |
-: unknown.
RB/LB: right and left breast
Regarding aetiology, it is clear that the actual causes of IPs in men are unknown. There are several conditions suggested as potentially responsible for the development of IPs in men, although nothing has been unequivocally proved. Gynaecomastia, misuse of anabolic steroids (through the consequent gynaecomastia or not) [10], increased serum prolactine levels [5], phenothiazine therapy (which is known to increase prolactine levels) and prolonged phenothiazine treatment [8] have all been reported as triggering factors for the development of IPs in the male breast. There is also a report of a case of an 11-year-old boy with in IP, after partial excision of a malignant brain tumour, following radiotherapy and chemotherapy [9].
The average age of the men with IPs is 39 (11–71). The majority of IPs in men has bloody nipple discharge as presenting symptom and they are not painful or sensitive to palpation. Diagnosis is confirmed through excision and histologic examination of the specimen and there was only one case where core biopsy was used preoperatively. The excisional biopsy is also sufficient treatment for the IPs in men. In the case reported by Gaurav et al., an IP in a 52-year-old man was not initially removed and progressed to invasive ductal carcinoma years later [5].
IPs in men are extremely rare and may be associated with medical treatments or hormonal abnormalities. They have the same clinical and radiological appearance as in women and a single duct bloody nipple discharge is the most common presenting symptom. Surgical excision is advisable, not only for diagnosis but as treatment too, as there is a chance for cancerous progression in a minority of cases.
Conflict of Interest statement
None declared.



