-
PDF
- Split View
-
Views
-
Cite
Cite
Tsukasa Nakamura, Kiyokazu Akioka, Shuji Nobori, Shumpei Harada, Norio Yoshimura, Hidetaka Ushigome, Upper extremity distal dual bypass enables arteriovenous fistula construction in a critical limb ischemia, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz022, https://doi.org/10.1093/jscr/rjz022
Close - Share Icon Share
Abstract
Arteriovenous fistula (AVF) trouble in a dialysis patient sometimes results in severe forearm ischemia.
We present the case of 27-year-old man with severe steal syndrome complained of AVF malfunction. There was a condition where an upstream artery of AVF is occluded and AVF is maintained by regurgitation from the palmar arch with ischemic digits. The patient underwent distal dual bypass: proximal to peripheral artery arterioarterial and arteriovenous bypasses and brachial arterioplasty. His skin perfusion pressure improved from 17 to 90 mmHg with enough quantity of blood: 250 ml/min for hemodialysis.
In severe steal syndrome cases, it is often observed that proximal artery is occluded and AVF inflow was supplied from palmar circulation and collateral vessels. Distal dual bypass is effective to re-establish digital circulation and repair AVF malfunction simultaneously in PAD patients.
INTRODUCTION
Peripheral artery disease (PAD) has increased as a serious problem in dialysis patients despite intensive focus having been paid to PAD [1]. Arteriovenous fistula (AVF) malfunction directly leads to poor hemodialysis efficiency and results in a variety of complications. In cases of irreversible AVF malfunction, surgical angioplasty is rarely performed. Instead of angioplasty, AVF reconstruction in the upper side is often performed. But this procedure would deteriorate ischemic changes in the extremities. Therefore, a distal dual bypass in an upper extremity (UE) has huge benefits for these patients with PAD in UE. However, a distal dual bypass in UE seems to be a minor procedure partially because of low popularity and technical difficulties. Thus, the aim of this report is to broaden the effectiveness of UE distal dual bypass to establish AVF reconstruction while securing digital circulation.
CASE REPORT
A 27-year-old male patient, underwent renal transplantation when he was 15-year old due to renal hypoplasia, but, was ultimately introduced hemodialysis. Following AVF construction, he experienced the steal syndrome, resulting in amputation of his left third digit and multiple AVF reconstruction. His left forearm AVF was malfunction due to severe PAD: quantity of blood flow was 70–110 ml/min because of complete obliteration of the proximal radial artery. Angiography demonstrated that obstruction of the proximal radial artery and regurgitation from the palmar arch to the AVF. This AVF condition barely enabled to perform daily hemodialysis with low efficiency with Kt/V < 1.0 (Daugirdas equation) [2] (Fig. 1). Exertional symptoms, tingling, and frigid digits were noted mainly due to decreased blood flow to the hand. The left second digits SPP was 17 mmHg. In order to restore digital circulation and AVF, distal dual bypass was planned under general anesthesia. First, in order to secure arterial inflow, brachial arterial stricture was excised and anastomosed end-to-end*. Following arterioplasty, however, the AVF flow measured by the doppler US, was still too weak to maintain hemodialysis. Thus, subsequently, the patient was given 5 000 units of intravenous heparin totally and monitored by ACT testing: 150–200. Regarding proximal anastomosis of the first distal bypass, the left brachial artery (distal to the * anastomosis) and reversed GSV graft were anastomosed with interrupted 7-0 prolene suture. In terms of the distal side, the posterior wall was sutured by parachute anastomosis technique, and the anterior wall anastomosis with interrupted 8-0 prolene was performed. Next, because it is true that AVF in the distal forearm is generally recommended, to repair forearm AVF, the second distal bypass was performed. The proximal portion was created at the proximal radial artery, downstream from the first distal bypass in order to prevent secondary steal syndrome. The left radial artery and reversed GSV graft were anastomosed with interrupted 7-0 prolene suture. Regarding the distal end side, the GSV graft and cephalic vein were sutured by the parachute anastomosis technique with 7-0 prolene. Finally, regurgitation from the palmar arch was ligated. The first distal bypass graft blood flow was 36 ml/min, measured by VeriQ (Medistim, Oslo, Norway). Angiography demonstrated satisfied simultaneous palmar arch and AVF circulation (Fig. 2). The left second digits SPP improved to 90 mmHg following reflow. Kt/V improved to1.53 (Daugirdas equation) with well-maintained AVF. The both graft patency was confirmed without any endovascular intervention at 12-month following distal bypass.
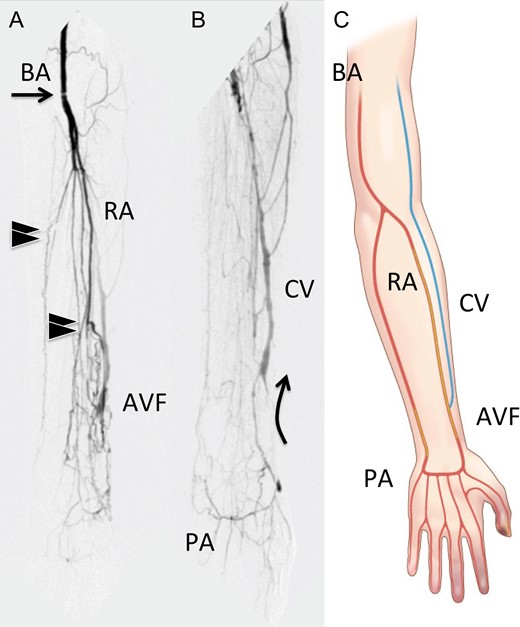
(a) The early phase of pre operative angiography shows that brachial artery stenosis (arrow), multiple arterial occlusions in the forearm (black arrowheads). (b) The late phase of pre operative angiography demonstrates steal syndrome: palmar arch to arteriovenous fistula blood flow (arrows). (c) Schematic presentation of ischemic upper extremity. BA, brachial artery; RA, radial artery; CV, cephalic vein; PA, palmar arch; AVF, arteriovenous fistula.
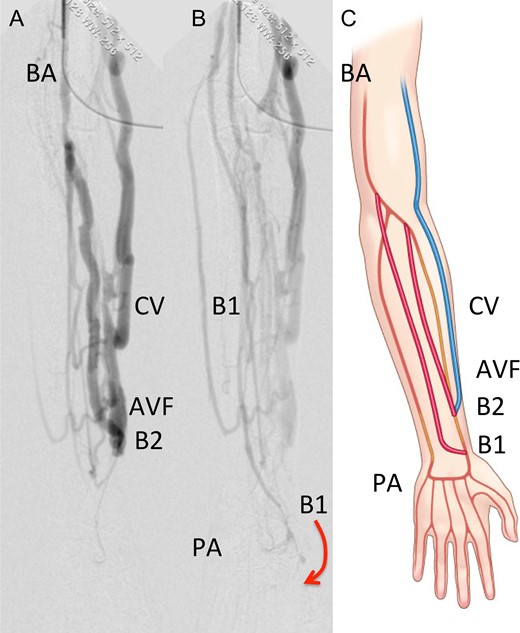
(a) The early phase of post-operative angiography shows enough blood flow in arteriovenous fistula. (b) The late phase of post-operative angiography demonstrates arterioarterio distal bypass to re-vascularize digital circulation. Arrow indicates the direction of blood circulation. (c) Schematic presentation of distal dual bypass BA, brachial artery; B1, the first bypass (arterioarterio bypass); B2, the second bypass (arteriovenous bypass); CV, cephalic vein; PA, palmar arch; AVF, arteriovenous fistula.
DISCUSSION
UE distal bypass has still not gained popularity, because it is technically difficult, and UE PAD is relatively rare. Conversely, there are patients who require digital revascularization, for instance patients on hemodialysis with an inappropriate AVF condition [3]. Although management of patients on hemodialysis has improved, there is an increasing number of patients with AVF trouble, partially because of an increase in the absolute number of hemodialysis patients and an aging population. Generally, aggressive surgical repairs, including distal bypass, seem to be avoided. Alternatively, patients are often referred for AVF reconstruction in the upstream, dominant side or for catheter hemodialysis. Nevertheless, it can be argued that distal dual bypass can be applied in UE when a patient requires the establishment of both peripheral circulation and AVF simultaneously. In more detail, this distal dual bypass could restore AVF with proximal arterial obstruction and peripheral regurgitation, as in the presented case. In order to rescue the digital circulation, the first distal bypass should be as far as possible from the proximal side and revascularize angiosome well-oriented peripheral artery. The second bypass acts as a substitute for the occluded artery. Importantly, it is better to intercept the communication between the AVF and palmar circulation like as distal revascularization and interval ligation (DRIL) [4] (Fig. 3). Furthermore, in order to prevent steal syndrome, an independent distal dual bypass would be ideal: the proximal side of the arterial bypass is located upstream compared to that of the AVF. However, from the aspect of vein graft sparing for future troubles, there seems to be disadvantages in the use of independent dual vein grafts. Thus, it is of vital importance to find the shortest courses of a dual bypass to establish blood circulation. Generally, AVF construction is recommended in and around the wrist [5], because of the low complication rates and preservation of the UE vein. In fact, well-maintained AVF is the ‘Achilles’s heel’ of patients on hemodialysis. The efficacy of hemodialysis is directly linked to the outcomes [6]. Distal dual bypass has the possibility of improving the limb/AVF condition and Kt/V, even in patients with severe PAD. Given these facts, AVF reconstruction in the forearm would also be recommended and justified by applying the distal bypass procedure. A limitation of the distal dual bypass in UE would be its ineffectiveness for patients with severe digital artery disease. However, as a future perspective, distal bypass combined with regenerative medicine would be a promising procedure as a multidisciplinary therapy even for these severe PAD cases.
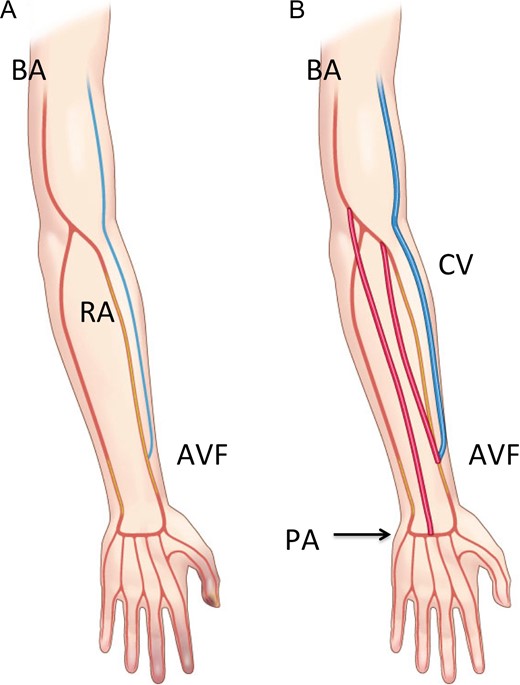
Schematic presentation of distal dual bypass in upper extremity to establish re-vascularization in hands and arteriovenous fistula. BA, brachial artery; RA, radial artery; CV, cephalic vein; PA, palmar arch; AVF, arteriovenous fistula.
CONCLUSION
It can be argued that distal dual bypass is a useful procedure to re-establish peripheral blood circulation and AVF in patients with AVF malfunction in an ischemic limb.
Acknowledgments
T.N. thanks Kyoto Prefectural University of Medicine Hospital C5 ward staffs who care the patient.
Conflict of Interest statement
None declared.
Funding
None.



