-
PDF
- Split View
-
Views
-
Cite
Cite
Jeong-moh John Yahng, Toan Pham, The tales of two neighbours: when cholecystitis does not preclude pancreatitis, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz019, https://doi.org/10.1093/jscr/rjz019
Close - Share Icon Share
Abstract
An 83-year-old lady with no previous history of gallstones, presented with a sudden-onset severe epigastric pain radiating through to the back associated with nausea and vomiting. On examination, the patient’s vital signs were normal. There was severe epigastric tenderness on palpation, as well as moderate right upper quadrant tenderness. Serological investigations showed raised inflammatory markers and serum lipase of 13 000, confirming the diagnosis of acute pancreatitis. Liver function tests were mildly deranged with a normal bilirubin of 12 μmol/L. An abdominal ultrasound demonstrated a distended gallbladder with multiple subcentimeter gallstones and diffuse wall thickening up to 7 mm, consistent with cholecystitis. A follow-up CT abdomen demonstrated evidence of pancreatitis with moderate peripancreatic fat stranding. The diagnosis of concomitant acute cholecystitis and gallstone pancreatitis was made based on the radiological and biochemical findings. The patient underwent an uncomplicated laparoscopic cholecystectomy. The histopathology confirmed cholelithiasis with acute on chronic cholecystitis.
INTRODUCTION
Cholelithiasis is a common condition, occurring in 10–15% of the population in developed countries, and up to 20% of these present as acute calculus cholecystitis [1]. Acute pancreatitis is also a common condition, with annual incidence worldwide of 4.9–73.4 cases per 100 000 people [2], and of these gallstone pancreatitis makes up ~50% of the cases, followed closely by alcohol induced pancreatitis [3]. Although being the two commonest gallstone-related conditions, these cholecystitis and pancreatitis rarely occur concurrently, [4, 5] thus there are only limited reports in the literature. Nevertheless, recent pathological and radiological studies have demonstrated their concomitant occurrence may be much higher than thought to be [4, 6]. The authors believe that the majority of the concomitant cases may be subclinical. We herein present a case of concurrent acute pancreatitis and calculous cholecystitis in a patient whose predominant pathology was pancreatitis. The patient was successfully treated with inpatient laparoscopic cholecystectomy after supportive management of acute pancreatitis.
CASE REPORT
An 83-year-old lady with a past medical history of ischaemic heart disease, asthma, hypertension and ex-tobacco smoking, presented to emergency department with a sudden-onset severe epigastric pain. The pain was described by the patient as burning in nature and radiated through to the back, and was associated with nausea and vomiting. On examination, the patient’s vital signs were normal. There was severe epigastric tenderness on palpation, as well as moderate right upper quadrant tenderness.
Serological investigations showed elevated white blood cell count of 12.6 × 109/L and C-reactive protein of 170. Moreover, the serum lipase was 13 000, confirming the diagnosis of acute pancreatitis. Liver function tests were mildly deranged but with a normal bilirubin of 12 μmol/L, ALT of 92 U/L, AST of 146 U/L, ALP of 89 and GGT of 117 U/L.
An abdominal ultrasound (Fig. 1) demonstrated a distended gallbladder with multiple subcentimeter gallstones. There was diffuse gallbladder wall thickening up to 7 mm and associated probe tenderness, consistent with cholecystitis. The common bile duct diameter measured up to 7.4 mm without any evidence of choledocholithiasis, thus did not require ERCP. However, the pancreas was not well visualized. A follow-up CT abdomen (Fig. 2) was performed, which demonstrated evidence of pancreatitis with moderate peripancreatic fat stranding without any features of complications including necrosis, abscess or pseudocyst.
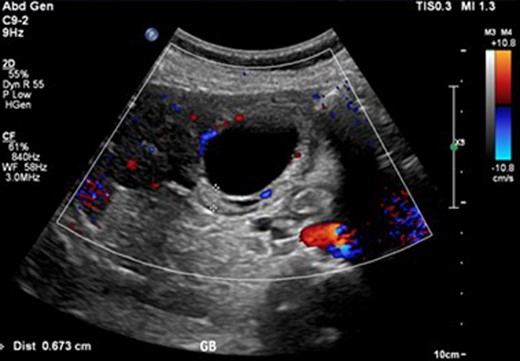
Ultrasound image of cholecystitis demonstrating thickened gallbladder wall.

The diagnosis of concomitant acute cholecystitis and gallstone pancreatitis was made based on the radiological and biochemical findings.
The patient underwent an uncomplicated laparoscopic cholecystectomy following successful conservative management of both cholecystitis and pancreatitis. The histopathology confirmed cholelithiasis with acute on chronic cholecystitis.
DISCUSSION
Despite their ubiquitous occurrence individually, acute cholecystitis and pancreatitis are seldom encountered concomitantly in clinical practice. This may be explained by the size disparity between the larger gallstones required to cause cholecystitis versus those that are small enough to pass through into the common bile duct to cause pancreatitis.
However, a histological study by Hung et al. [4] demonstrated that in 31 cases of gallstone pancreatitis that had cholecystectomy, the histopathology revealed cholecystitis with varying degrees of gallbladder wall inflammation. In addition, the study by Coffey et al. [7] revealed that 33 out of 184 cases of acute pancreatitis had concomitant histological evidence of cholecystitis. Of these 33 cases, 22 were chronic and 11 were acute. Of the 11 cases of acute type, 3 had serious complications of acute cholecystitis, where 2 developed gallbladder perforation and 1 with a pericholecystic abscess [7].
Despite the irrefutable histological evidence of concomitant acute cholecystitis in one-third of the cases of gallstone pancreatitis in Coffey et al. [7], from the authors’ experience, some of the histological acute cholecystitis may be subclinical. In our case, the patient’s principal presenting complaint was of pancreatitis with epigastric pain and elevated lipase, and cholecystitis was only revealed on ultrasound when abdominal ultrasound demonstrated sonographic features of acute cholecystitis with focal probe tenderness of the gallbladder. Working out the degree of correlation between histological cholecystitis and clinically significant cholecystitis will require further studies.
It is evident that even when there is clinically significant cholecystitis associated with pancreatitis, the prognosis for pancreatitis in such cases is good as this form of pancreatitis is usually the oedematous variety that is mild in severity [8]. The treatment of choice for cases of dual pathology is cholecystectomy which also prevents further episodes of gallstone pancreatitis. It was previously thought that cholecystectomy favourably influences the course of acute pancreatitis when occurred as a concomitant of acute calculous cholecystitis [8, 9]. However, more recent studies have demonstrated that early surgical intervention during the acute inflammatory phase of pancreatitis should be avoided due to high morbidity and mortality associated SIRS [10] as well as pancreatic oedema impairing Calot’s triangle dissection [5].
Therefore, the progress of the acute cholecystitis should be closely followed, and the timing of cholecystectomy should be dictated by the predominating pathology between acute cholecystitis and pancreatitis, and cholecystectomy should be delayed until clinical improvement of pancreatitis unless evidence of sepsis from cholecystitis [7].
The predominating pathology in the current case was the acute pancreatitis, hence, cholecystectomy was delayed until the clinical improvement of the pancreatitis, with the acute cholecystitis component adequately temporized with intravenous antibiotic.
CONCLUSION
Concurrent cholecystitis and gallstone pancreatitis are infrequently encountered in clinical practice. Despite the sparse reporting in the literature, the authors believe that the incidence may be higher than initially thought due to the subclinical nature of these cases. The treatment of choice is cholecystectomy, and the timing of cholecystectomy should be delayed, when possible, until the clinical improvement of the pancreatitis. However, the timing of cholecystectomy should ultimately be dictated by the more predominating pathology between cholecystitis and pancreatitis.
Conflict of Interest statement
None declared.
References
- pancreatitis, acute
- pancreatitis
- cholecystitis, acute
- cholecystitis
- inflammatory markers
- bilirubin
- chronic cholecystitis
- epigastric pain
- biliary calculi
- follow-up
- liver function tests
- palpation
- diagnosis
- gallbladder
- laparoscopic cholecystectomy
- nausea and vomiting
- vital signs
- serum lipase level result
- gallstone pancreatitis
- abdominal ultrasonography
- abdominal ct
- cholelithiasis
- histopathology tests
- right upper quadrant of abdomen



