-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroto Kitahara, Naohisa Wakabayashi, Hayato Ise, Chiharu Tanaka, Sentaro Nakanishi, Natsuya Ishikawa, Hiroyuki Kamiya, Open brachiocephalic artery stent for static obstruction caused by acute type A aortic dissection, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz018, https://doi.org/10.1093/jscr/rjz018
Close - Share Icon Share
Abstract
Brachiocephalic artery dissection complicated by acute type A aortic dissection occasionally causes cerebral malperfusion. Although immediate central aortic repair has been the standard treatment for aortic dissection, dissection in supra-aortic vessels frequently remains after the surgery. The residual brachiocephalic artery dissection is reported to be associated with late neurological events. Therefore, additional intervention for brachiocephalic artery dissection during central aortic repair should be considered in selected cases. In this report, we describe two cases requiring open brachiocephalic artery stenting simultaneous with central aortic repair. There were no neurological or stent induced complications at latest follow-up.
INTRODUCTION
Brachiocephalic artery dissection is caused by extension of acute type A aortic dissection into the supra-aortic vessels. Although the preoperative brachiocephalic artery dissection is associated with increased mortality in patients undergoing central aortic repair, there is no definitive treatment indication for brachiocephalic artery dissection at the time of the surgery. In this report, we describe two cases of brachiocephalic artery dissection complicated by acute type A aortic dissection. The static obstruction in the brachiocephalic artery was detected during the surgery and successfully treated with open brachiocephalic artery stenting simultaneous with central aortic repair.
CASE REPORT
Case 1
An 86-year-old woman with acute type A aortic dissection was transferred to our institution. Contrast enhanced computed tomography (CT) showed aortic dissection involving the ascending aorta extending to the proximal descending aorta. The true lumen of the brachiocephalic artery was occluded by the false lumen (Fig. 1). No neurological symptoms were present preoperatively. The patient was transferred to the operating room, and underwent central aortic repair with ascending aortic and bicaval cannulations. Cerebral perfusion was monitored with near-infrared spectroscopy (INVOS cerebral oximeter, Somanetics Inc, Troy, USA) and transcutaneous carotid echo. Inside the aorta, the orifice of the brachiocephalic artery was completely occluded by the false lumen. Selective cerebral perfusion (SCP) through the brachiocephalic artery was initiated immediately, however, the SCP flow was not sufficient due to stenotic lesion with low right side regional oxygen saturation (rSO2). Considering low rSO2, it was felt that the lesion should be treated even without preoperative neurological symptoms. The S.M.A.R.T. Vascular Stent System (Cordis Corp, Fremont, CA, USA) (12 mm × 40 mm) was inserted and deployed inside the brachiocephalic artery. After SCP cannula was inserted through the stent, right side rSO2 increased similar to the left side. Finally, ascending aortic replacement by using 26 mm J-Graft (Japan Lifeline Co., Ltd., Tokyo, Japan) was performed. Postoperative course was uneventful without any neurological event. Postoperative CT scan showed good stent patency and no residual dissection in the brachiocephalic artery (Fig. 2).
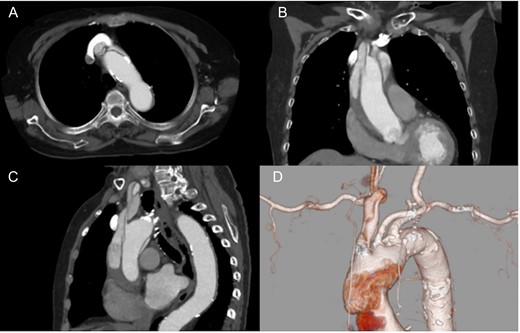
Preoperative computed tomography findings. Axial (A), coronal (B) and sagittal view (C). 3D computed tomography angiography (D). The brachiocephalic artery was occluded by the false lumen.
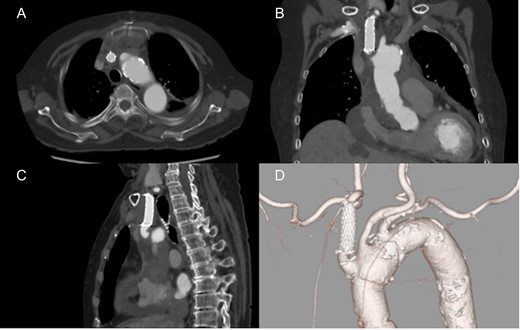
Postoperative computed tomography showing patent carotid stent and no residual dissection. Axial (A), coronal (B) and sagittal view (C). 3D computed tomography angiography (D).
Case 2
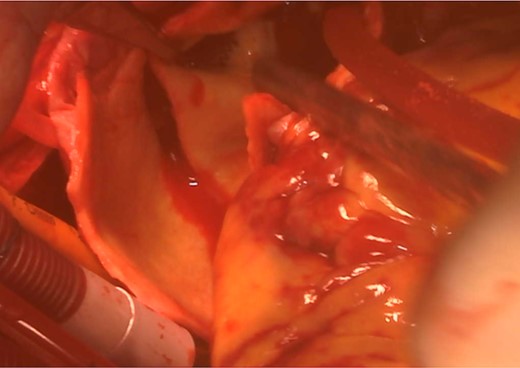
An 82-year-old woman with loss of consciousness was transferred to our institution. CT showed aortic dissection involving ascending aorta extending to the brachiocephalic artery where the true lumen was occluded due to the false lumen. The level of consciousness was getting improved during examination, then, the decision was made to proceed with performing central aortic repair first. Cardiopulmonary bypass was established with ascending aortic and bicaval cannulations. Through the surgery, rSO2 was continuously within normal range bilaterally. Incising the aorta, the tear was located in the ascending aorta and the brachiocephalic artery was severely compressed by the false lumen. Then, the lesion was expanded and stabilized with the S.M.A.R.T. stent (10 mm × 40 mm) (Fig. 3). Finally ascending aortic replacement by using 26 mm J-Graft was done. The neurological status was clear after the surgery. There were no neurological or stent induced complications at discharge and the most recent follow-up.
DISCUSSION
Brachiocephalic artery dissection extended from acute type A aortic dissection was reported to be an independent risk factor of perioperative cerebral malperfusion, which resulted in increased mortality [1]. Immediate central aortic repair has been a standard treatment for acute type A aortic dissection, even with neurological symptom due to cerebral malperfusion [2]. However, residual dissection frequently remains after central aortic repair without direct surgical or endovascular intervention to the brachiocephalic artery. Charlton-Ouw et al. [3] reported that untreated residual carotid artery dissection had a low risk of subsequent stroke or need for subsequent carotid revascularization. On the other hand, Neri et al. [4] reported that residual carotid artery dissection was associated with increased risk of late ischemic events. There has been no definitive indication of additional intervention for brachiocephalic artery dissection at the time of central aortic repair. Therefore, considering the balance between the risk of late ischemic event and intervention related complications, indication of brachiocephalic artery intervention should be discussed in a case by case basis.
There have been several case reports describing endovascular interventions for residual carotid artery dissection complicated with late ischemic event [5] or false lumen aneurysmal formation [6]. In our cases, preoperative CT scan showed brachiocephalic artery occlusion due to the dissection. Inside the aorta, the brachiocephalic artery was severely compressed by the false lumen, then it was thought to be static obstruction, which frequently remains even after central aortic repair and causes cerebral malperfusion or late neurological events. To prevent the perioperative or future neurological complications, we decided to perform open brachiocephalic artery stenting simultaneous with central aortic repair. To our knowledge, there has been only one case report performing open stenting for the carotid artery dissection. It was used to reinforce the fragile intima of dissected carotid artery with spiral form tears inside [7]. Another reason we performed open brachiocephalic artery stenting was low rSO2 value during SCP detected by INVOS. The cerebral monitoring devices are useful to assess adequate cerebral perfusion and help to decide the need for additional intervention [8]. Even though case 1 patient did not complain any neurological symptoms preoperatively, brachiocephalic artery intervention should be considered when the rSO2 was low without any known reasons. Furthermore, once the open brachiocephalic artery stent was deployed, it allowed easy insertion of SCP and hold the SCP cannula very steadily.
In conclusion, we performed open brachiocephalic artery stenting for static obstruction due to acute type A aortic dissection. We believe that open brachiocephalic artery stenting is easy and quick procedure, and it would be beneficial in selected patients. Cerebral monitoring may give us useful information to decide if performing brachiocephalic artery intervention during central aortic repair.
Acknowledgements
None.
Conflict of Interest statement
The authors declare that they have no competing interests.
Funding
None.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient for this publication.



