-
PDF
- Split View
-
Views
-
Cite
Cite
Randa Ghazal Asswad, Anna Harrison, Paul S Hans, Casandra Buzatu, Laryngeal ulceration in Behçet’s disease: the role of centres of excellence in the UK, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz017, https://doi.org/10.1093/jscr/rjz017
Close - Share Icon Share
Abstract
Behçet’s disease (BD) is a rare complex multisystem inflammatory condition characterized by the triad of symptoms: aphthous ulcers of the mouth and genitalia and uveitis.
We present the case of a 31-year-old Caucasian male who had a prolonged journey from first presentation until diagnosis of BD. For 11 years, he presented symptoms affecting the oral cavity and oropharynx, with worsening odynophagia and dysphagia and ultimately, development of stridor. Flexible laryngoscopy showed significant laryngopharyngeal ulceration and scarring. Treatment was with colchicine, corticosteroids and azathioprine and supervised by one of three newly established BD Centres of Excellence in the UK.
Although uncommon, ENT manifestations in patients with BD should be taken into consideration to allow for early recognition and treatment of what can become a life-threatening condition. In such situations, early referral to a BD Centre of Excellence is essential to provide confirmation of diagnosis and supervision of treatment.
INTRODUCTION
Behçet’s disease (BD) is a rare complex multisystem inflammatory condition that involves both arterial and venous blood vessels. The condition was first identified in 1937 by Dr Hulusi Behçet, a Turkish Professor of Dermatology, who described a triad of symptoms: aphthous ulcers of the mouth and genitalia and uveitis [1]. It is a chronic relapsing disease involving multiple organs that affects people typically between 25 and 40 years of age.
While oral ulcers are common and characteristic of BD, the literature details only few reports of laryngeal ulceration. In those cases, their potential for significant oedema of that region results in a risk of airway obstruction [2, 3]. This article describes the case of a patient with laryngeal ulceration secondary to BD, with diagnosis only occurring late in the course of the disease which had likely been present for many years.
CASE REPORT
We present the case of a 31-year-old Caucasian man with a history of recurrent mucosal ulcerations of the mouth and larynx for 11 years. The first presentation of his condition was to an Ear, Nose and Throat (ENT) department, aged 20, for severe odynophagia. Clinical examination and investigation at that time revealed a 1 cm ulceration of the oropharynx. A biopsy was performed, which showed a non-specific inflammatory infiltrate. The patient received conservative treatment and was discharged. Over the next 10 years, he was admitted twice to the ENT department for severe odynophagia, once with stridor due to supraglottic oedema with a partial response to corticotherapy.
The clinical history and examination revealed the presence of recurrent oral ulcerative lesions (Fig. 1a and b) that developed in crops and lasted up to several weeks, with ulcerative lesions on the epiglottis and the left aryepiglottic fold (Fig. 2) and another lesion on the rectal mucosa. Biopsies taken from both lesions showed non-specific inflammatory infiltrates, with a predominance of neutrophils. The patient also reported papular skin lesions and pathergy following blood tests (Fig. 1c).
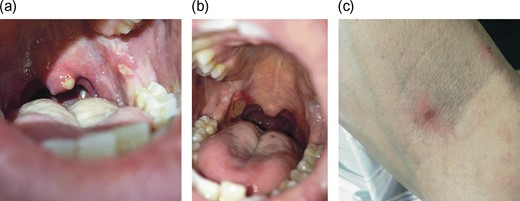
(a and b) Numerous painful ulcers of the oral cavity overlying the uvula, retromolar trigone and soft palate. (c) Papular skin lesions suggesting positive pathergy.
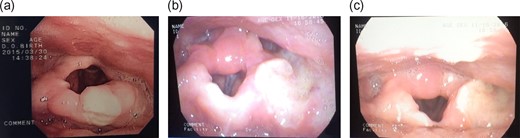
Flexible laryngoscopy demonstrated general oedema and distortion of the supraglottis. (a) An initial ulcerative lesion on the epiglottis. (b and c) Ulceration on the left aryepiglottic fold extending laterally into the left pyriform sinus. There is oedematous swelling of the arytenoids, but the vocal folds were found to be normal. There is subsequent scarring of the epiglottis following healing of the initial epiglottic ulcer.
The differential diagnosis at that stage included multiple aetiologies. Infectious causes, were excluded by biopsy and negative tests for bacteria (e.g. tuberculosis) and viral infections (HIV, Herpesviridae viruses). The patient was screened for malignancy by blood tumour markers and imaging, which were negative. An autoimmune work-up, including ANA, dsDNA, p-ANCA, c-ANCA, Ro, La antibodies were all negative.
Considering the presence of recurrent oral ulcerations and excluding neoplastic and infectious causes, the possibility of BD was entertained, and the patient was referred to one of the UK Centres of Excellence for BD.
At that time, the patient did not meet the formal classification criteria for BD, but he was closely monitored and received treatment with colchicine and low dose corticosteroids, with symptomatic benefit. In time, he developed genital ulcers and several deep vein thromboses (despite appropriate anticoagulant treatment), thus fulfilling the requirements according to the International Criteria for Behçet’s Disease (ICBD).
Treatment included immunosuppression with azathioprine, colchicine and low dose cortisone therapy to minimize the recurrence of ulcerations, to which the patient responded well.
DISCUSSION
Reaching a diagnosis of BD can be challenging, both as it is a rare disease and there is no single test that can confirm or exclude it. A positive diagnosis, therefore, relies on the presence of appropriate clinical symptoms and signs, with the exclusion of all other causes such as infection, malignancy or an autoimmune disorder.
There are various classification criteria for BD, reflecting the difficulties in diagnosis. Published in 1990, the International Study Group for Behçet’s Disease (ISGBD) criteria is the most widely accepted and commonly used approach in diagnosis [4] (Table 1). In 2006, new criteria were developed with the hope of obtaining a better specificity and sensitivity in diagnosis, the ICBD [5] (Table 2). This case eventually scored positively against both.
| Recurrent oral ulcers . |
|---|
| Plus, any two of the following: |
| Recurrent genital ulcers |
| Eye lesions |
| Skin lesions |
| Positive pathergy test |
| Recurrent oral ulcers . |
|---|
| Plus, any two of the following: |
| Recurrent genital ulcers |
| Eye lesions |
| Skin lesions |
| Positive pathergy test |
| Recurrent oral ulcers . |
|---|
| Plus, any two of the following: |
| Recurrent genital ulcers |
| Eye lesions |
| Skin lesions |
| Positive pathergy test |
| Recurrent oral ulcers . |
|---|
| Plus, any two of the following: |
| Recurrent genital ulcers |
| Eye lesions |
| Skin lesions |
| Positive pathergy test |
| Symptom . | Points . |
|---|---|
| Oral ulcers | 2 |
| Genital ulcers | 2 |
| Ocular manifestations | 2 |
| Positive skin pathergy test | 1 |
| Skin lesions | 1 |
| Neurological manifestations | 1 |
| Vascular manifestations | 1 |
| Symptom . | Points . |
|---|---|
| Oral ulcers | 2 |
| Genital ulcers | 2 |
| Ocular manifestations | 2 |
| Positive skin pathergy test | 1 |
| Skin lesions | 1 |
| Neurological manifestations | 1 |
| Vascular manifestations | 1 |
A score ≥ 4 points is needed for a diagnosis of BD.
| Symptom . | Points . |
|---|---|
| Oral ulcers | 2 |
| Genital ulcers | 2 |
| Ocular manifestations | 2 |
| Positive skin pathergy test | 1 |
| Skin lesions | 1 |
| Neurological manifestations | 1 |
| Vascular manifestations | 1 |
| Symptom . | Points . |
|---|---|
| Oral ulcers | 2 |
| Genital ulcers | 2 |
| Ocular manifestations | 2 |
| Positive skin pathergy test | 1 |
| Skin lesions | 1 |
| Neurological manifestations | 1 |
| Vascular manifestations | 1 |
A score ≥ 4 points is needed for a diagnosis of BD.
However, it must be borne in mind that these are classification, not diagnostic, criteria and are best considered as guidelines. As this case reveals, initial symptoms can appear many years before formal diagnosis, when the patient finally fulfils all of the necessary criteria for a positive diagnosis due to the staggered presentation of symptoms and signs. In addition, the fact that this patient presented with potentially life-threatening severe involvement of the larynx is concerning.
A systematic review by Webb et al. [6] highlighted the ENT manifestations of BD. There are few case reports of patients with BD developing ulcerations that extended down into the larynx, thus causing acute laryngeal inflammation and oedema, with risk of airway obstruction, and subsequent scarring [3]. A recent report from Ireland suggests destructive laryngeal disease in BD may actually be more prevalent than was previously thought, and the authors highlight that this can even occur in otherwise clinically asymptomatic patients [2]. Additionally, BD has been associated with an increased risk of pharyngeal stenosis, variable sensorineural hearing loss and vestibular dysfunction [6].
The aim of treatment in BD is to prevent exacerbations and irreversible damage that can impact on quality of life. BD is treated according to the European League Against Rheumatism recommendations that were last updated in 2018 [7]. Treatment is decided based on the organ system involved and severity. For less complex mucocutaneous disease, a first line regimen of oral colchicine with topical steroids is normally recommended. Azathioprine, oral steroids, mycophenolate or tacrolimus can also be added, with infliximab used for the most resistant cases.
This case highlights that although uncommon, ENT manifestations in patients with BD should be considered and patients screened, with particular attention to the larynx, to allow for early recognition and treatment of what can become a life-threatening condition. In such situations, referral to an appropriate expert BD multidisciplinary team, as has developed in three national Behçet’s Syndrome Centres of Excellence across the UK [8], is essential to provide confirmation of diagnosis and supervision of treatment, which may involve biological therapies. By providing a ‘one-stop’ service, these centres are able to offer the best available treatment and the holistic approach to care needed. This case provides awareness for surgical teams that newly established centres exist to help in such complex cases.
Acknowledgements
The authors would like to thank Professor Robert Moots (Professor of Rheumatology at the University of Liverpool and Director of the National Centre of Excellence for Behçet’s syndrome, Liverpool, UK) for his help and expertise within this field.
Conflict of Interest statement
None declared.
Funding
This work received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- colchicine
- azathioprine
- patient referral
- behcet syndrome
- adrenal corticosteroids
- deglutition disorders
- ulcer
- glucocorticoids
- cicatrix
- genitalia
- mouth
- oropharynx
- aphthous stomatitis
- uveitis
- european continental ancestry group
- diagnosis
- hypopharynx
- mineralocorticoids
- swallowing painful
- stridor
- flexible laryngoscopy
- professional supervision
- laryngeal ulcer



