-
PDF
- Split View
-
Views
-
Cite
Cite
Sardar Hassan Arif, Ayad Ahmad Mohammed, Esophageal stricture as a complication of stent placement for leak after sleeve gastrectomy, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz353, https://doi.org/10.1093/jscr/rjz353
Close - Share Icon Share
Abstract
Obesity is defined as body mass index (BMI) greater than 30. Weight loss improves the quality of life and alleviates or even treats some obesity-related comorbidities with general improvement in the quality of life. Sleeve gastrectomy results in major reduction of the size of the stomach and decreases the sense of hunger due to various hormonal and neuronal pathways. A 31-year-old lady had BMI of 49 underwent sleeve gastrectomy. Three weeks after surgery, she presented with epigastric pain and vomiting with radiological signs of leak. Endoscopic esophageal stent placed with resultant improvement of the condition; after stent removal, she developed esophageal stricture diagnosed with barium study. The patient underwent repeated successful endoscopic dilatation. Leak and bleeding are the most serious complications after sleeve gastrectomy. Subclinical leak is treated with antibiotics, drainage of the collection and stent, critical patients need stenting with operative repair of the site of leak.
INTRODUCTION
The awareness about obesity and obesity-related morbidity is increased in the population; there are many methods for weight reduction like dietary restrictions, exercise, medications and weight reduction surgeries, i.e. bariatric surgeries [1].
Obesity is defined as body mass index greater than 30. Weight loss improves the quality of life and alleviates or even treats some obesity-related comorbidities such as diabetes, hypertension, joint problems, sleep disturbances, improve the body self-esteem and results in a general improvement in the quality of life [1, 2].
There are two types of bariatric surgical procedures, restrictive and malabsorptive types; in the first type, there is restriction of the capacity of eating like the sleeve gastrectomy, and in the second type, the absorption of the nutrients from the bowel is reduced like many types of the bypass procedures. Some procedures are purely restrictive, some are purely mal-absorptive and some are combined [1–3].
Sleeve gastrectomy, sometimes called longitudinal or vertical sleeve, was first introduced as a modification of the biliopancreatic diversion that is combined with duodenal switch in 1998 and was performed laparoscopically for the first time in 1999 [4].
This procedure involves resection of the stomach alongside a bogie which is inserted through the mouth to about 5–6 cm from the pyloric ring resulting in major reduction of the size of the stomach and decrease the sense of hunger due to various hormonal and neuronal pathways [2].
CASE PRESENTATION
A 31-year-old lady with body mass index of 49 presented for weight reduction surgery after failed other attempts like dietary restrictions and regular exercise. The patient was otherwise health with negative past medical and surgical histories.
Sleeve gastrectomy was done for her with uneventful intraoperative and postoperative periods. After 3 weeks from the surgery, she presented with epigastric pain and repeated attacks of vomiting, which was little amount and containing pus. She was admitted to the hospital and send for computed tomography (CT) scan of the chest and abdomen, which showed no intra-abdominal or intrathoracic collections. She received proton pump inhibitors and oral antibiotics with some improvement; after 10 days, she presented with the same complaint, CT scan was repeated, which showed localized collection at the region of the cardia with extravasation of the oral contrast.
Endoscopic esophageal stent placed for 2 months, with improvement of the clinical condition; after stent removal, she presented with dysphagia, barium study showed esophageal stricture at the middle third of the esophagus at the site of the upper margin of the stent (Fig. 1).
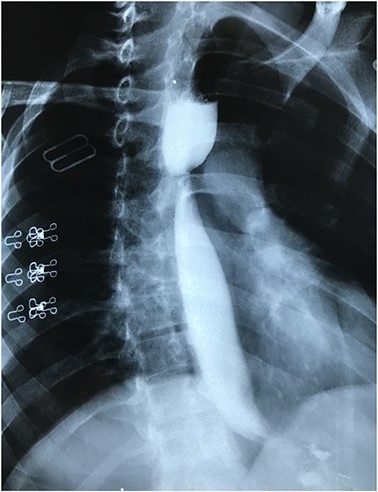
Barium study showing stricture at the middle third of the esophagus with proximal dilatation.
The patient underwent repeated endoscopic dilatation with successful dilatation at the end of the management (Fig. 2).
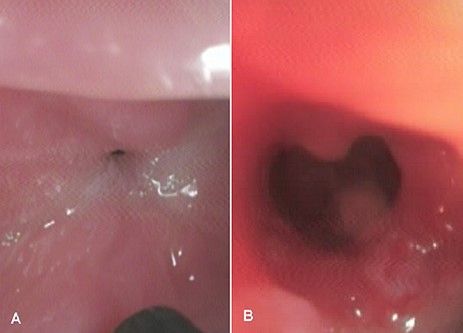
An endoscopic view showing (A) esophageal stricture before endoscopic dilatation, and (B) the site of the stricture after successful endoscopic dilatation.
Barium study repeated after the endoscopic dilatation, which showed passage of the contrast agent to the stomach with no evidence of stricture (Fig. 3).
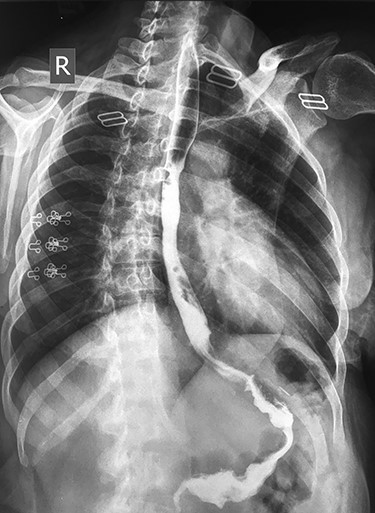
Barium study showing the passage of the contrast agent to the sleeved stomach with no evidence of stricture after successful endoscopic dilatation.
DISCUSSION
Most patients experience excellent weight loss after sleeve gastrectomy, and many authors proved that sleeve gastrectomy can be used as a single procedure for weight reduction [4].
To improve the success of this this type of surgery, the patient selection criteria should include the weight, the dietary habits of the patient, the types of the foods mostly consumed, the personality pattern of the patient, the presence or absence of endocrine disorders and psychiatric disorders should be excluded [1].
Laparoscopic sleeve gastrectomy is a relatively safe procedure, but it may be associated with some complications such as bleeding, leak from the site of the staple lines, reflux, prolonged vomiting, nutritional deficiencies and stricture [2, 5].
Leak is the most serious complication, which is estimated to complicate up to 5% of cases of sleeve gastrectomy. Leak is generally classified by two classifications, the first one is depending on the radiological appearance and clinical features in which it is divided into type I (subclinical leak) when the leak is minimum and localized and the patient is stable clinically and type II (clinical leak) when there is free intraperitoneal leak in which the patient has major clinical deterioration, and the second classification is depending on the time of the leak, which divides it into acute leak if occur less than 3 days and chronic if occur after 8 days [2, 5].
When the leak is subclinical, it is usually treated with antibiotics, drainage of the collection and sometimes stent placement, patients presented with clinical leak need operative intervention such as stenting and repair of the site of leak [2].
Strictures may occur acutely after surgery due to edema, which are usually treated with supportive care, and it resolves in the majority of the patients or later on due to inflammation or ischemia, which needs more complex interventions such as endoscopic management or even surgical intervention [2].



