-
PDF
- Split View
-
Views
-
Cite
Cite
Ameer Kakaje, Firas Al Khoury, Ammar Alfarroukh, Lina Khouri, Familial sliding hiatus hernia in four siblings with uncommon features: a case series report, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz318, https://doi.org/10.1093/jscr/rjz318
Close - Share Icon Share
Abstract
This case report shows a very rare case series of one family with four children who had severe congenital sliding hiatus hernia (HH) with uncommon presentations, and they had one parent with sliding hernia and the other with reflux symptoms. It is rarely described in the literature a direct link to a familial type that might refer to a common genetic factor. Hiatus hernia is protrusion of abdominal viscera through the oesophagus opening in the diaphragm into the thoracic cavity with sliding hernia being the most common. It can be either asymptomatic or accompanied by a variety of symptoms. We present a case series of one family in which four siblings had congenital sliding diaphragmatic hernia with atypical symptoms and gastro-oesophageal reflux disease (GORD). It is a rare case that suggests a common factor that can cause such a common disease. All four had uncommon presentations which all required surgical repair. Few cases reported on the medical literature, and they were discussed and compared with our case. However, we need further studies in families that might have this phenomenon.
INTRODUCTION
A hiatus hernia (HH) occurs when the viscera of the abdomen protrude through the oesophageal hiatus to the thoracic cavity [1]. HH is not commonly seen among the paediatric age group, and it is asymptomatic most of the time. However, it may vary in symptoms and complications [2], with regurgitation being the most common in the first year of life [3]. In this case series report, we describe four siblings (see Fig. 1) who had HH with their lower oesophageal sphincter (LES) locating above the diaphragm. They were born from a father with gastro-oesophageal reflux disease (GORD) without HH and the mother with asymptomatic HH with reflux (see Fig. 2). The parents were fourth-degree-related. Three of the children had symptomatic sliding diaphragmatic HH with uncommon presentations and the other child with a more advanced hernia. The patients did not have pulmonary hypoplasia, and there was a positive history in two siblings of the father (out of five) who had small symptomatic hiatus hernia and a negative history from the mother. The parents had four affected children in addition to one child who died from pneumonia at 2 years of age.
CASE REPORTS
Case 1
A 30-month-old girl suffered from melena and coffee ground vomiting for a year. She suffered from oesophageal stricture which was dilated twice but with recurrence. She had microcytic anaemia (Hb: 6.5 g/dl). The barium meal showed a type 4 HH which was repaired with Nissen in open surgery resulting in her becoming symptom-free.
Case 2
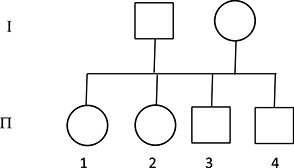
Numbered cases: sorted from older to youngest: (1) A 30-month-old girl with melena, coffee ground vomiting and severe anaemia. (2) A 38-month-old girl with epigastric pain, appetite loss and mild anaemia. (3) An 18-month-old boy with pallor and severe anaemia. (4) An 8-month-old boy with melena with no anaemia.
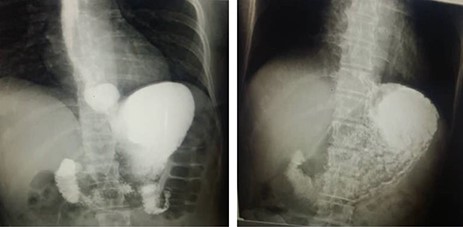
Parents’ barium swallow: (1) It shows on the left the asymptomatic hiatus hernia of the mother with reflux. (2) It shows on the right a reflux with the father who was symptomatic with no hernia.
A 38-month-old girl was admitted with 2-week history of epigastric pain and 10-day history of appetite loss. Labs showed normal CBC with a slight anaemia (Hb: 11.9 g/dl). Endoscopy showed a displacement of the LES with a stricture in the lower third. The barium meal showed the abdominal viscera protruding into the chest with left mediastinal displacement (see Fig. 3). Open surgery showed stomach protrusion into the thoracic cavity which was fixed in the abdominal cavity with diaphragm repair.
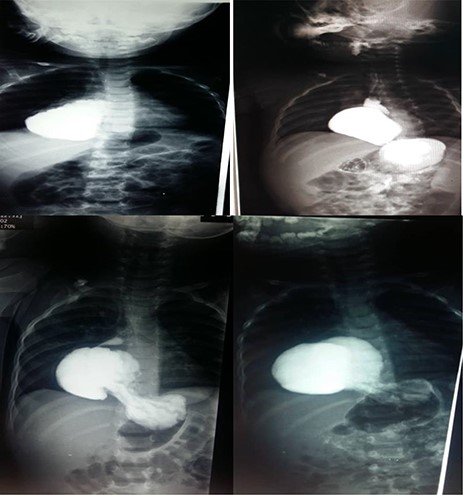
Upper left photo is of case two that shows a barium swallow with 5.5 cm hiatus hernia. The upper right photo is of case 4 that shows a barium swallow with 8 cm hiatus hernia. Lower 2 photos are of case 3 that show barium swallow with a 6 cm hiatus hernia.
Case 3
An 18-month-old boy was admitted to the Children Hospital with a 3-week history of progressive pallor and 1 day history of melena after which his parents brought him to a private clinic when a chest X-ray showed that he had HH with the stomach being in the chest cavity with an enlarged left pulmonary hilum and right mediastinum displacements (see Fig. 3). CBC showed that he was also severely anaemic (Hb: 6 g/dl). He reported no other symptoms and had not been prescribed any previous medications. An endoscopy was performed which showed an abnormal location of the stomach in the thoracic cavity. The barium meal was obtained which confirmed the HH. In open surgery from the abdomen, the stomach and the oesophageal hiatus were found to be herniated into the thoracic cavity. They were repaired with Nissen surgery.
Case 4
An 8-month-old boy was admitted with a 20-day history of black, loose diarrhoea (5–6 occurrences in total) with no frank blood in the stool. He had low fever. Lab tests were normal with positive stool occult blood test. Following symptomatic treatment for 2 weeks, an endoscopy was conducted which showed a displacement of the LES with mild lower ulcerative oesophagitis and was confirmed later on with a plain X-ray and a barium meal to be an 8 cm HH (see Fig. 3). The HH was repaired with Nissen open surgery.
DISCUSSION
Familial clusters with hiatal hernias have been described in a few studies [4–8], most fully by Carre et al. It described one family with 38 members in 5 generations, 23 members of them had been confirmed by radiology to have a hiatal hernia. Every affected member had an affected parent while having a male-to-male transmission. This case reported by Carre et al., in addition to our case, proposes a dominant mode of inheritance, but Carre et al.’s report did not describe the symptoms of GORD [4]. In the case series reported here, we can observe in the family tree that four children have inherited more severe forms of sliding hernia from their father with much more severe symptoms. In the four cases presented in this paper, much more than 2 cm separation between the LES and the diaphragmatic hiatus in the radiographs raised the consideration of a sliding HH.
The indication for anti-reflux surgery is not indicated for only having a sliding hiatus regardless of having a large HH, although large HH is often associated with severe reflux symptoms, poorer treatment response, and erosive oesophagitis [9]. However, when GORD and a sliding hernia are found together, anti-reflux surgery is indicated [10]. HH can be massive, causing strangulation, anaemia and severe bleeding in addition to breathlessness and thoracic pain [2, 8].
This study is one of the few studies suggesting a genetic or familial factor which can cause a congenital HH. We still need more studies to better understand this phenomenon.



