-
PDF
- Split View
-
Views
-
Cite
Cite
Sam Alhayo, Michael Devadas, Laparoscopic sleeve gastrectomy following multiple failed endoscopic sleeve gastroplasties, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz315, https://doi.org/10.1093/jscr/rjz315
Close - Share Icon Share
Abstract
Endoscopic sleeve gastroplasty (ESG) is a new obesity control modality. Limited data are available to describe post ESG findings and approaches to surgically revise this procedure. Two female patients with persistent obesity despite multiple ESG procedures underwent laparoscopic sleeve gastrectomy (LSG). Pre- and post-ESG, LSG body mass index (BMI), weight, and excess weight loss percentage (EWL%) were recorded. Endoscopic findings and revisional LSG technique were carefully documented. Pre-ESG BMI of the patients were 44 and 52 kg/m2. Pre-LSG BMI were 44.6 and 50 kg/m2. Pre-LSG gastroscopy and laparoscopy revealed complete dehiscence of ESG sutures with full-thickness invasion of these sutures and titanium clips through the gastric wall and some intraperitoneal adhesions. At 7-month follow-up, BMI are 40.3 and 35.7 kg/m2 and EWL% are 39 and 43%, respectively. This is the first study reporting LSG following failed ESG. ESG can lead to significant complications. LSG is achievable post-ESG and has superior results to it.
INTRODUCTION
Obesity is an increasing burden on modern society. Nearly 300 million people in the western world are diagnosed with body mass index (BMI) >30 kg/m2 [1]. The annual costs of obesity and its complications are forecasted to double in the following two decades [1].
Multiple surgical and endoscopic procedures have been developed to achieve the best outcomes with the least complications.
Bariatric surgery is the most effective treatment for obesity. It is associated with successful long-term maintenance of weight loss and reduction in obesity-related morbidities. It is also associated with the improvement of patients’ quality of life [2].
Laparoscopic sleeve gastrectomy (LSG) is the most popular bariatric procedure. However, endoscopic techniques, such as endoscopic sleeve gastroplasty (ESG), are being introduced as equivalent to surgical options in obesity control.
ESG is a relatively new modality advocated for patients with a BMI of 30–40 [3]. Data are limited in describing post-ESG findings or approaches to surgically revise this procedure.
CASE REPORT
Two patients underwent multiple endoscopic bariatric procedures in 2016–2017. LSG was performed in 2018.
Patient 1, a 30-year-old female, had a BMI of 44. She underwent endoscopic intragastric balloon inflation in 2015, ESG in 2016, and then repeated in 2017. Patient 2, a 32-year-old female, had a BMI of 51 kg/m2. She, similarly, underwent repeated ESGs in 2016 and 2017. Repeat procedure was performed due to poor weight control and persistent metabolic derangement in the second patient.
The endoscopic treatments were performed by the same endoscopist, and it involved performing gastroscopy during which three rows of full-thickness sutures were placed along the greater curvature of the stomach using the Overstitch (Apollo Endosurgery) and additional four mattress sutures were placed to re-enforce the suture line. Further sutures were used to capstone the stitches within the fundus. The resultant gastric volume was described to be 25% of pre-ESG size. All procedures were reported to have no immediate complications. Patients were discharged on the same day. Both were instructed to remain fasted for 2 days during which they received IV fluid infusions in an outpatient clinic. Clear fluids were then permitted for 3 days, followed by free fluid diet for a month.
Patient 1 had a maximum weight loss of 9 kg and a BMI drop to 40.8. This was shortly gained back to reach a BMI of 44.6 before her LSG. Patient 2 lost a maximum of 20 kg and dropped her BMI to 43.1. However, she also shortly gained back her weight to reach a BMI of 50 kg/m2.
Both patients sought surgical opinion 1 year later due to weight re-gain after the end of the liquid diet phase and complaints of vague abdominal pain.
Gastroscopy was performed 2 weeks pre-surgery and revealed complete dehiscence of ESG sutures (Figs 1 and 2). All visible sutures and clips were removed endoscopically.

Endoscopic view during gastroscopy showing dehiscence of endoscopic sleeve gastroplasty sutures. This was taken 2 weeks prior to laparoscopic sleeve gastrectomy
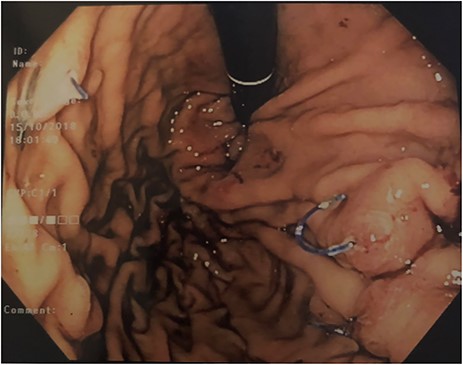
Retroflexed endoscopic view during gastroscopy showing dehiscence of endoscopic sleeve gastroplasty sutures. This was taken 2 weeks prior to laparoscopic sleeve gastrectomy
Laparoscopic findings during LSG revealed invasion of endoscopic suturing material and titanium clips eroding through the gastric wall, with intraperitoneal adhesions (Figs 3 and 4).

Laparoscopic view during sleeve gastrectomy reveals full-thickness invasion of endoscopic sutures and titanium clips through the gastric wall
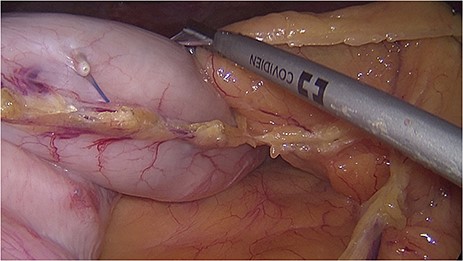
Laparoscopic view during sleeve gastrectomy reveals full-thickness invasion of endoscopic sutures and titanium clips through the gastric wall
Division of adhesions and removal of invading ESG hardware had to be done first. The stomach was mobilized, and gastric tube was created using multiple firings of articulated laparoscopic stapling device. The staple line was imbricated. Cardiopexy and omentopexy were performed. Drain was inserted but shortly removed post-operatively after normal swallow study. These were performed due to the high risk of leak in these patients.
The most recent 7-month post-operative follow-up revealed a BMI of 40.4 and 35.7 kg/m2 and TBWL% of 20.2 and 19.9%. Patients’ excess weight loss percentage are 39 and 43%, respectively.
DISCUSSION
Many weight-control approaches are being developed. These ultimately aim for easier reproducible technique, low complication rate, and better obesity control.
ESG had gained attention for its advertised minimal invasiveness, quicker recovery, and low or nil complications [4]. It involves the creation of gastric tube through plication of gastric mucosa using an Overstitch device. It is reported to be a less invasive intervention with equivalent outcomes to surgery for patients with BMI < 35 kg/m2. Some authors reported total body weight loss of up to 20.9% over 24 months in one series [5].
Despite the low risk advertised with ESG, major post-procedure complication rates are reported between 1.1 and 2.4%, and procedure failure ranges between 50 and 90% [5, 6].
The minimal invasiveness of ESG can cause a dilemma as physicians may get lured for repeat procedures when failure occurs. ESG has also got comparable operative time to LSG [6] which is raising anesthetic concerns due to the risks associated with prolonged endoscopy [7].
In a recent study, ESG was performed under laparoscopic view, during which endoscopic suturing of the gastric wall to the anterior abdominal wall had occurred inadvertently [8]. This was similarly observed in the two cases described above raising suspicion of post ESG peri-gastric leak as well. The hardware invasion of the gastric wall and their removal are problematic due to the potential risk of suboptimal staple line outcome in LSG.
A comparative study between ESG, LSG, and gastric band found that LSG achieved the highest TBWL% after 6 and 12 months. The peri-gastric leak rate for LSG was reported to be similar to ESG [2].
Major complications of LSG included gastric staple line leaks in the past. With the improvement of staplers and techniques, the rate of leak dropped to < 1% in the 2016/2017 Bariatric Surgery Registry Report [9].
In the discussed cases, patient selection for ESG was concerning as both patients had BMI > 40 kg/m2. Also, patients underwent multiple repeated endoscopic interventions with likely peri-procedural complications. These were symptomized through abdominal pain and were eventually confirmed laparoscopically.
To our knowledge, this is the first case report describing LSG following failed ESG. It also demonstrates trans-gastric suturing of the stomach to abdominal wall during ESG.
ESG is a novel procedure that should provide good obesity outcomes with minimal complications in selected patients. However, this procedure, in our experience and through systematic review, has comparable complication rates and operative time to LSG with poorer weight loss outcomes than previously reported. It is also a demanding procedure with a steep learning curve [10]. Careful training and patient selection are mandatory to achieve better results. Further high-quality studies are recommended to compare outcomes between ESG and LSG.
ACKNOWLEDGEMENTS
Verbal and written consent were obtained from both patients for publishing purposes of this case report and for follow-ups.
Conflict of interest statement
None declared.



