-
PDF
- Split View
-
Views
-
Cite
Cite
Saira Nisar, Jeffrey L Roberson, Taryn E Travis, Laura S Johnson, Jeffrey W Shupp, Extensive hidradenitis suppurativa with dorsal foot involvement: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz349, https://doi.org/10.1093/jscr/rjz349
Close - Share Icon Share
Abstract
Hidradenitis suppurativa (HS) is a highly morbid chronic inflammatory skin disease resulting in painful and purulent lesions classically occurring in areas with a high density of apocrine glands such as the groin and axillae. This is the case of a 53-year-old male with medically refractory Hurley stage III HS affecting multiple anatomical sites including the dorsum of the right foot, an atypical location. Throughout his hospital course, he underwent a series of surgical excision and graft procedures to treat extensive HS lesions on various anatomical locations. In patients with a history of HS, mechanical stress may result in atypical lesion locations. In addition to the standard medical and surgical treatment, management should include optimizing nutritional parameters, smoking cessation, wound care and reducing friction and pressure at the affected area.
INTRODUCTION
Hidradenitis suppurativa (HS) is an inflammatory skin disease characterized by recurrent painful and exudative lesions in regions with a high density of apocrine glands, classically intertriginous areas. Despite an estimated prevalence of 0.05–4.10% of the population [1] and significant morbidity, the exact pathophysiology remains unclear. Likely a multifactorial disease, social factors such as smoking, obesity, low socioeconomic status, family history of HS and bacterial colonization are all hypothesized to be involved in the development of the pathology [2]. While there is no consensus on a treatment modality that maximizes disease free time, oral antibiotics can be attempted for isolated nodules and inflammation (Hurley stage I) with surgical excision being considered for singular tract formation (Hurley stage II) and coalescing tracts with fibrosis (Hurley stage III) [2,3,4].
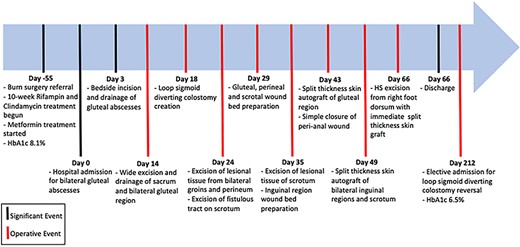
Timeline from first encounter with the burn surgery service to completion of surgical procedures.
This is a case of a patient with longstanding HS involving multiple anatomical locations, including an atypical presentation on the dorsum of the right foot. He underwent extensive medical and surgical management with a hospital course lasting longer than 2 months.
CASE REPORT
A 53-year-old male with a 4-year history of HS requiring antibiotics, surgical excision and complex wound closure presented with multiple new draining tracts with purulence along the perineal and gluteal folds (Hurley stage II), leading to pain on sitting and lying on the back. Furthermore, he had extensive
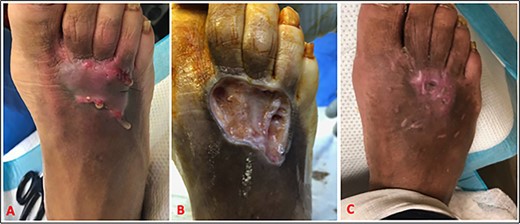
(A) HS on dorsum of the right foot. (B) HS lesion excised to the subcutaneous tissue. Immediate split-thickness skin graft (not shown). (C) Near complete wound healing by postoperative day 17.
of the inguinal folds and scrotum. He also reported a 1-week history of small abscesses with purulent drainage at the dorsum of the right foot with surrounding cellulitis and hypertrophic scar. His only other complaint was slow weight loss over the last year due to malnourishment. He worked as a maintenance employee and reported a long history of cigarette smoking, which was stopped 2 weeks prior to presentation. On exam, he was afebrile with leukocytosis of 23 k/uL with neutrophilia. On this occasion, he was also diagnosed with diabetes mellitus with HbA1c of 8.1%, for which metformin was prescribed. Burn surgery was consulted and thereafter took over care, due to the extensive HS involvement of the skin and anticipated complex surgical excision and grafting. Initially, he was discharged home with an increase in metformin dose, a 10-week course of rifampin and clindamycin, zinc supplements, in addition to education on appropriate nutritional intake.
Eight weeks later, he returned to the emergency room with increased pain and drainage from the bilateral gluteal abscesses. He underwent incision and drainage in addition to treatment with the aforementioned antibiotics. At this time, his disease was upstaged to Hurley stage III. Due to the refractory nature of his disease, he subsequently underwent a series of surgical procedures to remove the bulk of the offending tissue, divert his fecal stream and definitively close the wounds on his bilateral groin, gluteal region, perineum, scrotum and right foot (Fig. 1). A loop sigmoid colostomy was performed as part of the management for diversion of the fecal stream was created to allow healing of the sacral and perianal region.
For the dorsal foot HS, he underwent excision and immediate split-thickness skin graft (Fig. 2). Histological analysis of the foot HS skin biopsy showed thicker epidermis and irregular rete ridges compared with normal skin biopsy taken from the unaffected leg. Furthermore, there was an increased cellular infiltrate in the dermis of the HS skin compared with normal skin due to inflammation (Fig. 3).
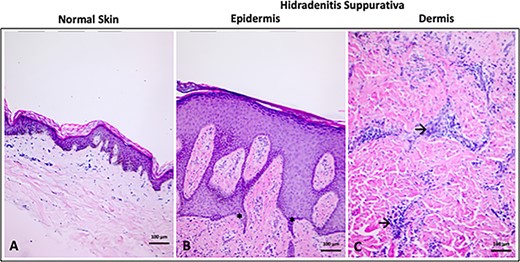
(A) Normal skin epidermis and dermis. (B) Thicker epidermis and increased irregularity of rete ridges (*) in HS. (C) Cellular infiltrate in HS dermis (→). Hematoxylin and eosin stain. Scale bar = 100 μm, 10× magnification.
A multidisciplinary team comprising of burn surgeons, a wound care nurse specialist, a nutritionist and occupational and physical therapists were involved in the care of this patient. Overall treatment goals were to optimize nutrition for adequate wound healing, improve mobility, encourage smoking cessation, establish strict glycemic control and improve quality of life. Furthermore, he was advised on appropriate footwear to offload pressure and reduce friction to prevent future pedal lesion formation. On follow-up, his surgical wounds were healing; his glycemic control improved (HbA1c = 6.5%), and he had optimum nutritional parameters. He continues to attend outpatient wound clinic and is recovering well.
DISCUSSION
HS is an inflammatory skin disease of unknown etiology; however, smoking, obesity and diabetes are implicated in disease severity [1, 5]. Smoking alters the body’s inflammatory response and sweat gland activity and releases toxins in the sweat, which can exacerbate HS. Poor glycemic control, along with smoking, hinders the body’s wound healing ability, further complicating and prolonging recovery after surgery [5].
While recurrent palmoplantar hidradenitis has been reported as a rare pediatric condition [6, 7], there is only one other documented case of HS of the dorsal aspect of the foot in an adult [8]. These cases hypothesize that in a population predisposed to infundibular hyperkeratinization and follicular dilatation, mechanical and/or thermal trauma can cause interfollicular hyperplasia and follicular rupture, resulting in the HS inflammatory response. This patient’s extensive history of HS necessitating antibiotics and surgical excision combined with the mechanical stress due to his occupation could have predisposed to the development of his pedal lesion. Thus, management of similar patients should include appropriate footwear and strategies to reduce mechanical stress.
CONCLUSION
Severe cases of HS require multiple surgical procedures leading to prolonged hospital stay and recovery time. The authors recommend a multidisciplinary approach for management of HS to achieve disease control and improve quality of life for these patients. Particular aims should be to reduce the modifiable risk factors such as smoking cessation, adequate nutritional status and strict glycemic control.
Conflict of Interest statement
None declared.



