-
PDF
- Split View
-
Views
-
Cite
Cite
Minas Kostis, Vasileios Patriarcheas, Stamatios Apergis, Michail Leontis, George Panayiotakopoulos, Isolated pneumomediastinum following laparoscopic cholecystectomy: a rare complication, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz340, https://doi.org/10.1093/jscr/rjz340
Close - Share Icon Share
Abstract
Development of postoperative pneumomediastinum is one of the most infrequent complications of laparoscopic procedures. We report a case of a 47-year-old woman who developed pneumomediastinum consequently to laparoscopic cholecystectomy. The patient was treated conservatively and was discharged on the fifth postoperative day. Early detection of this condition, differential diagnosis and careful monitoring of the patient are important, as it may lead to severe consequences, including the life-threatening tension pneumomediastinum.
INTRODUCTION
Laparoscopic cholecystectomy is considered to be the gold standard for the treatment of symptomatic cholelithiasic disease. It is a safe and cost-effective procedure, with a major decrease in hospital stay, sick leave and postoperative complications in comparison with open surgical methods. However, it is not a completely risk-free procedure. Its most common complications include the following: bile duct injury, perforation of the gallbladder, bile leaks, bleeding and bowel injury [1].
Pneumomediastinum is a clinical entity characterized by the presence of air in the mediastinal cavity. It is a rare complication following laparoscopic abdominal surgery with only one case of isolated pneumomediastinum having been reported in the past [2].
We present a case of pneumomediastinum following laparoscopic cholecystectomy, in a patient with symptomatic cholelithiasic disease.
CASE REPORT
The patient is a 47-year-old woman who presented with acute upper abdominal pain radiating to the right scapula. She had recurrent episodes of postprandial right quadrant discomfort, for a year. Six months ago, an abdominal ultrasound was performed, which showed microlithiasis and sludge in the gallbladder. She was thus instructed to follow a low-fat diet.
An ultrasound was performed upon admission, which showed multiple gallstones within the gallbladder.
Nonsteroidal anti-inflammatory medication was administered, which alleviated the symptoms.
Laboratory tests (hematological, biochemical, coagulation) were normal.
Taking into consideration the patient’s history and the risk of complications, such as cholecystitis, cholangitis, pancreatitis etc., it was decided to proceed to laparoscopic cholecystectomy on the following day.
Carbon dioxide was used for the insufflation of the peritoneal cavity, as it is nonflammable, has higher blood solubility than air, reducing the risk of gas embolism and is a normal metabolic end product, rapidly cleared from the body. An infundibular approach was used, with dissection of the hepatobiliary triangle, clipping of the cystic artery and of the cystic duct. Surgery was performed as planned, and no intraoperative complications were observed. During the first postoperative day, our patient complained of shortness of breath, precordial pain and nausea. Pulse oximetry revealed reduced oxygen saturation (92%).
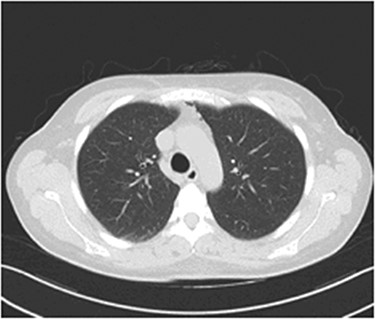
The possibility of pulmonary embolism was put first on the differential diagnosis list. In order to exclude this life-threatening complication, D-dimers and computed angiography of the pulmonary arteries were performed. Computed Tomography of the Pulmonary Arteries (CTPA) (Fig. 1) showed normal contrast enhancement of the pulmonary arteries, with no contrast deficits. Nevertheless, it brought out the presence of gas inside the mediastinum (capnomediastinum). Consequently, the D-dimers came out negative.

CTPA images show the presence of gas in the upper anterior mediastinum.
Our patient was put under oxygen therapy (Venturi 50%). As a precaution, antibiotic therapy was administered (teicoplanin/metronidazole), in order to prevent mediastinitis. During the second postoperative day, the clinical presentation of our patient was improved. The following day, the Venturi mask was replaced with a nasal cannula. In the fourth postoperative day, a computed tomography (CT) of the thorax was performed (Fig. 2), which showed a reduction of the amount of the air in the mediastinum, in concordance with the improvement of the clinical presentation of the patient. During the last day of hospitalization, the patient had no respiratory pathology symptoms, her clinical presentation was even more improved and she was discharged from the hospital on postoperative day 5.
Thorax CT during the fourth postoperative day: a significant reduction of the mediastinal gas collection is observed.
DISCUSSION
Pneumomediastinum (or mediastinal emphysema) is defined as the migration of air or other gas inside the mediastinal space. As a clinical entity, it was first described by Laennec—the inventor of the stethoscope—in 1819, as a consequence of traumatic thoracic injury [3].
Spontaneous pneumomediastinum was described 120 years later, in 1939 by Hamman, whose name was given to the hallmark sign of this condition. The pathophysiology of the condition depends on the clinical circumstances under which it is encountered. In general, pneumomediastinum can be divided into two categories: one in which the condition arose without an external causative factor and is referred to as spontaneous pneumomediastinum, and a second one known as secondary pneumomediastinum, which can be attributed to an external cause, such as trauma (blunt or penetrating injuries to the thorax and the abdomen), underlying pulmonary disease, such as asthma, chronic obstructive pulmonary disease, bronchiectasis, inhalation of toxic fumes or iatrogenic intervention including intubation, endoscopic procedures, etc. [4].
There are some factors that are thought to predispose to spontaneous pneumomediastinum (in which the air usually derives from ruptured alveoli located near the hilum of the lung), including tobacco and recreational drug use. Pneumomediastinum is usually a relatively benign condition, and only in a few cases, it can lead to severe complications. Notwithstanding its rareness, tension pneumomediastinum is a critical situation that may lead to diminished cardiac output, either due to direct cardiac compression (cardiac tamponade) or due to reduced venous return, as well as to airway compression. Tension pneumomediastinum would require Video-Assisted Thoracoscopic Surgery (VATS) or even thoracotomy to be handled. In addition, some cases of pneumomediastinum are further complicated by the coexistence of pneumothorax or extensive subcutaneous emphysema or even expand to the retropharyngeal space [5].
Pneumomediastinum following laparoscopic surgery in general is an extremely rare complication with only few cases reported in the past. In these cases, pneumomediastinum was reported with a combination of other complications such as gas-related subcutaneous emphysema or pneumothorax [6]. Isolated pneumomediastinum following laparoscopic cholecystectomy is considered to be a very rare event with only one report published in the literature [2]. In our case, it is hard to determine the exact way of the CO2 migration to the mediastinal space, taking into account that during the procedure there was neither perforation of the diaphragm nor barotrauma during the ventilation of the patient. After ruling out these two scenarios, we suggest the escape of insufflating gas into the retroperitoneal space and through anatomical pathways such as the aortic and esophageal hiatuses of the diaphragm.
In conclusion, isolated pneumomediastinum following laparoscopic cholecystectomy is considered to be very rare. The clinical suspicion of this unusual clinical entity has to be confirmed with radiological imaging. Monitoring and antibiotic therapy are sine qua non conditions for the prevention of serious life-threatening complications such as mediastinitis and cardiac tamponade.
Conflict of Interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
M. K. and V. P. collected the data and wrote the article, M. L. interpreted the data, S. A. critically revised the article and G. P. supervised the project and gave the final approval.



