-
PDF
- Split View
-
Views
-
Cite
Cite
Yaying Eileen Xu, Vinay Gounder, A rare case of multi-focal non-contiguous necrotizing soft tissue infections and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz338, https://doi.org/10.1093/jscr/rjz338
Close - Share Icon Share
Abstract
Necrotising soft tissue infection (NSTI) is a rare yet life-threatening surgical emergency, characterized by rapidly spreading infection below the epidermis to the soft tissue layers of the dermis, subcutaneous layers, fascia and sometimes muscle. Multi-focal NSTIs have been rarely described in the literature, with reported cases predominantly involving immunocompromised patients. We report a case of an immunocompromised 70-year-old woman who initially presented with concern of a perforated colonic malignancy requiring exploratory laparotomy and within 24 hours while on inotropes, developed rapidly progressing necrotizing fasciitis (NF) of the left thigh with renal failure secondary to sepsis. Despite aggressive debridement, a progress computed tomography later showed multi-focal non-contiguous necrotising myositis of the whole left lower limb and right gluteal regions. Early diagnosis of multi-focal NF especially in immunocompromised patients, repeat assessment, aggressive surgical debridement and prompt antibiotics usage are the key to treatment.
INTRODUCTION
Necrotising soft tissue infection (NSTI) a life-threatening infection of the soft tissues, characterized by subtle, rapid onset of spreading inflammation and necrosis which spreads along the deep fascia and occasionally involves underlying muscle, intense oedema and thrombosis of vessels running in the fascial sheaths lead to the necrosis of subcutaneous fat and overlying skin. The incidence rate is one in 100 000 with mortality rate between 40–70% [1]. The typical finding that should raise suspicion is severe pain that is disproportional to examination findings, accompanied by local oedema and erythema which can rapidly spread and lead to sudden clinical deterioration [2]. Multi-focal non-contiguous necrotizing fasciitis (NF) is extremely rare, and the atypical presentation involving multiple sites can be challenging and misleading for diagnosis and may lead to delay in management.
CASE REPORT
A 70-year-old woman presented to emergency with acute abdominal pain on a background of immunocompromised with type II diabetes and previous splenectomy secondary to trauma in 1980 and multiple previous laparotomies for adhesive bowel obstruction. Computed tomography (CT) abdomen raised the concern of a perforated splenic flexure malignancy (Fig. 1). She had laparotomy that showed grossly dilated large bowel with no obvious perforation; a loop colostomy was formed to decompress the large colon. Intravenous Piperacillin/Tazobactam was the initial antibiotic therapy, with vancomycin and fluconazole later added to cover possible micro-perforation. She was admitted to intensive care unit postoperatively due to ongoing shock and high vasopressor and noradrenaline requirement.

Significant inflammatory change surrounding an irregular appearing splenic flexure with the impression of a likely contained perforation in this region.
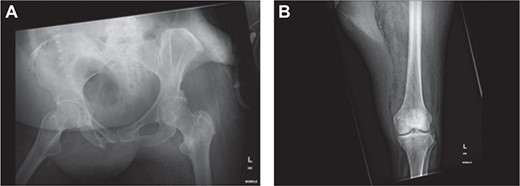
X-ray of (a) pelvis and (b) left lower limb demonstrated obvious air in soft tissue compartment in right gluteal and left thigh.
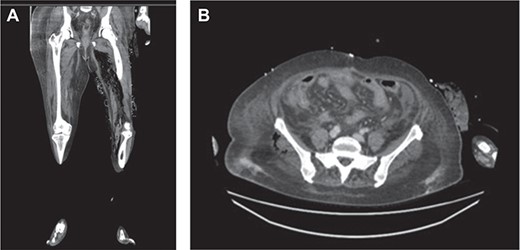
(a) Air in the deep medial and posterior compartments of the thighs and calf suggestive of residual infection in the deep compartment. (b) New finding of air in the right gluteus medius muscle.
Within 14 hours postoperatively, she developed an erythematous patch on her left thigh, and a creatine kinase of 19 000. A bedside finger test was performed which showed dirty dishwater fluid, necrotic fat and lack of bleeding. She was taken to theatre for urgent debridement for suspected NF. Antibiotics were changed to Meropenem, Vancomycin, Lincomycin and Fluconazole. She had extensive debridement of the soft tissue circumferentially on the left thigh, including some muscle. In 10 hours postdebridement, there was a radiological evidence of disease progression with gas in muscle compartments on the lower limb X-rays (Fig. 2a and b), and CT abdomen and lower limbs demonstrating gas throughout the whole left leg and a non-contiguous area in the right gluteal region (Fig. 3a and b). A diagnosis of multi-focal non-contiguous necrotising myositis was made.
Due to her multiple comorbidities and very high mortality risk with low risk of recovery to pre-morbid state, she was palliated in accordance with family wishes. Her swab and tissue microscopy unfortunately did not isolate a pathogen; this is likely due to early commencement of broad-spectrum antibiotics at admission.
DISCUSSION
NF can be classified into four types: type I, polymicrobial (at least one anaerobic species in combination with one or more facultative anaerobic species); type II, monomicrobial infection, most commonly by Group A Streptococci (less frequently other Streptococci or Staphylococci); type III, monomicrobial, usually Gram negative, including marine organisms; and type IV, fungal. The common sites of NF are the upper limb (10–48%), lower extremities (28%), perineum (21%) or trunk (18%), from which it expand to contiguous areas [2].
The laboratory risk indicator for NF (LRINEC) is scoring system based on six parameters that has been used to assist the diagnosis of NF. In a retrospective case series, patients with an LRINEC score of < 6, while unlikely to have NF, cannot exclude the possibility of the diagnosis [3]. Higher LRINEC scores are associated with higher mortality and amputation rates [3]. Imaging can contribute to the diagnosis of NF: inflammatory changes, collections from other sites and evidence of gas are seen on CT. However, gas on X-ray or CT is observed in only 17–29% of patients and it is a late sign. Magnetic resonance imaging is suggested to be the most adequate imaging to diagnose NF, but it is not readily available and not practical in an unstable patient [4]. Surgical exploration remains the gold standard to diagnose NF. The typical findings of finger test at bedside are necrotic tissues with a watery foul-smelling fluid described as ‘dishwasher’ fluid and the absence of bleeding. Early aggressive surgical debridement and broad-spectrum antibiotics are the keys in managing NF [4].
Multi-focal occurrence of NF in non-contiguous sites is extremely rare in the published literature. A recent review identified only 33 cases of multi-focal NF in the last 50 years [4]. The duration of delay in the appearance of secondary non-contiguous lesions ranged between a few hours and 3 days from the identification of the first lesion [4]. It was found that type II NF (52% of the cases) was most commonly associated with multi-focal NF. Type II NF is more aggressive in its progression, and with bacteremia and toxic-shock more frequently associated with type II disease, it may be inferred that septic embolization, hence multi-focal necrosis, is more likely to occur with a type II presentation than any other form of NF [5, 6]. Unfortunately, no micro-organism was identified in this patient due to early the use of broad-spectrum antibiotics.
A retrospective case-control study compared the characteristics of patients between multi-focal vs. unifocal NF; patients with multi-focal were more likely to have multiple comorbidities such as liver cirrhosis and end-stage renal disease. Immunocompromised patients have an increased risk of bacteremia, and their study showed that multi-focal NF patients (89%) had a much higher prevalence of bacteremia than mono focal NF patients (36%). The total case postoperative mortality rate was 68% in multi-focal NF as compared with 14% mortality with unifocal NF [7].
Frequent re-examination of a patient with NF is critical, and early imaging may play an important role in detecting subclinical multi-focal lesions [6]. The patient described in this case report had CT postinitial debridement which demonstrated the progression of disease of the ipsilateral side and new contralateral involvement. Unfortunately, with these new findings, the management plan was changed from further debridement to palliation. Early diagnosis especially in immunocompromised patients, repeat assessment, aggressive surgical debridement and prompt antibiotics usage are the key to treatment for multi-focal non-contiguous NF.
REFERENCE
- antibiotics
- sepsis
- computed tomography
- debridement
- dermis
- kidney failure
- epidermis
- necrotizing fasciitis
- immunocompromised host
- surgical procedures, operative
- thigh
- infections
- fascia
- leg
- colon cancer
- inotropic agents
- laparotomy, exploratory
- early diagnosis
- emergency surgical procedure
- soft tissue
- necrotizing soft tissue infections



