-
PDF
- Split View
-
Views
-
Cite
Cite
Luke D Hughes, Differential diagnosis for a ring-enhancing lesion on CT/MRI brain: retained cotton ball pledget, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz339, https://doi.org/10.1093/jscr/rjz339
Close - Share Icon Share
Abstract
New or persisting symptoms require careful evaluation and investigation. We present a case report of a 58-year-old man who underwent a craniotomy for a subdural haematoma and presented a decade later with worsening neurological symptoms. Investigation revealed the cause to be a delayed foreign body reaction to a retained cotton wool pledget.
INTRODUCTION
In neurosurgery, retained surgical material is relatively rare and yet it is notorious for causing diagnostic confusion. Retained surgical material can stimulate an immediate or a delayed reaction. The delayed reaction results in an inflammatory mass termed a gossypiboma, the effects of which may manifest many years later. In this case report is discussed the radiological appearances of retained surgical swabs and an explanation for the delayed presentation in a neurosurgical case.
THE CASE
A 58 year old gentleman presented in 2003 with headache, vomiting, collapse and new left-sided hemiparesis. A CT head scan revealed a right sylvian fissure and right frontoparietal subdural haematoma (SDH), with mass effect and mid-line shift. Initially this was evacuated via a burr-hole, followed by coil embolization of a ruptured right middle cerebral artery aneurysm. There was subsequent craniotomy for evacuation of a further SDH.
Post-operatively the left sided hemiparesis persisted and a dysaesthetic pain developed in the left upper and lower limbs. A CT scan revealed minimal residual clot, no hydrocephalus and a significant reduction in midline shift. The patient’s residual neurological symptoms were attributed to ischemic injury of the thalamus, internal capsule and basal ganglia.
At follow-up it was noted that the patient was experiencing headaches, had poor short-term memory and decreased sensation to the left side of his body. The hemiparesis persisted and a left upper motor neuron facial palsy was noted. In 2005 and in light of persisting symptoms, a follow-up CT scan was reported to show a small, hyper-dense cystic abnormality in the right external capsule (Fig. 1). It was postulated that the lesion was probably a calcified encysted haematoma, and the symptoms were attributed to post-stroke pain.
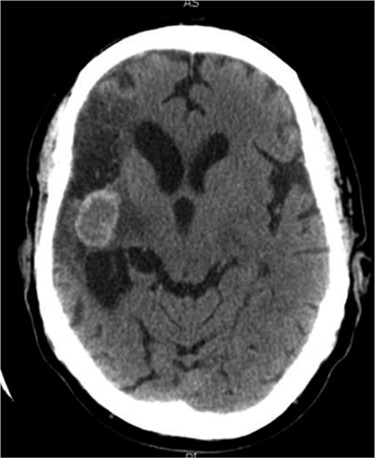
Axial CT head (2005) demonstrating hyper-dense cystic abnormality in the right external capsule.
Between 2005 and 2012, the clinical condition remained stable and there were no significant radiological changes identified (Fig. 2). In July 2012, the patient re-presented with worsening left sided weakness and a left sided homonymous hemianopia. CT scan at this time demonstrated a 4 × 4cm well-defined mass of CSF density in addition to the pre-existing lesion in the right external capsule. Neither enhanced with contrast and there was no significant midline shift. An MRI head showed the lesion to contain a significant solid component. It appeared somewhat vascular and there was suspicion that it could represent a low-grade tumour (Fig. 3). The patient underwent a right-sided craniotomy to remove the mass.

Axial CT head (2007) demonstrating hyper-dense cystic abnormality in the right external capsule.
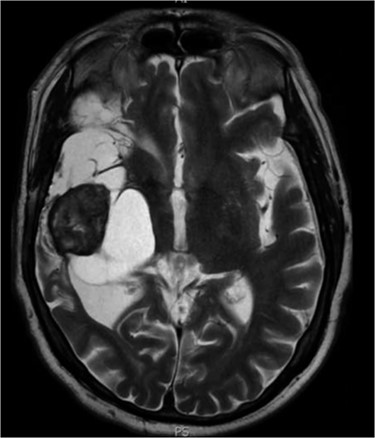
Axial MRI head (2012) demonstrating 4 × 4 cm solid mass with surrounding fluid enhancement.
Histological analysis showed large fragments of collagenous tissue. The central parts of the specimen had cholesterol clefts, macrophages and numerous foreign body type multinucleated giant cells. Vessels with calcified walls were also identified. The surrounding capsule contained reactive glial cells and vessels with perivascular inflammation. It was concluded that these findings were consistent with a marked foreign body response to a retained surgical swab.
DISCUSSION
The term ‘gossypiboma’ describes both the mass of retained surgical material and the associated inflammatory foreign body reaction [1]. Although rare, these carry important clinical and medico-legal ramifications.
To aid in differentiation most non-metallic equipment used in the theatre today contains a radio-opaque marker. Awareness of the radiographic appearance of these markers is required for detection and diagnosis. The typical findings of a gossypiboma on CT are of a soft tissue mass with internal gas bubbles, representing air trapped between the cotton fibres. Gas trapped between the threads of a surgical swab can last for weeks or months [2]. Upon magnetic resonance imaging, T2-weighted images appear as a mass with a hyper-intense centre and hypo-intense rim. With contrast-enhanced T1-weighted images, there is strong peripheral enhancement [3].
Retained foreign material tends to result in delayed healing. Patients may present with continued elevation of inflammatory markers and signs of local or systemic inflammation. Loss of function is one of the cardinal signs of inflammation. If the brain parenchyma is damaged and compressed by continued and expanding inflammation, an acute presentation might be expected. However, the brain and spinal cord are considered to be ‘immune privileged’ sites. They are separated from the rest of the body by the blood-brain barrier (BBB), which has highly selective permeability. One of the primary functions of the BBB is to prevent infections. It does so by inhibiting pathogen entry from the circulation into the central nervous system (CNS). However, the movement of antibodies, leukocytes, therapeutic and imaging agents may also be restricted [4, 5].
At peripheral sites, antigens are taken up by antigen presenting cells (APCs), wherein they are processed and presented on the cell surface attached to major histocompatibility complex (MHC) molecules, before being transported to local lymph nodes. However, in the CNS, APCs are not present in normal parenchymal tissue or the perivascular spaces. This is not to say that the CNS has no immune cells. Microglia are the resident macrophages of the brain and spinal cord and constitute 10–15% of the total glial cell population [6]. They are constantly scavenging the CNS for plaques, damaged neurons and infectious agents. Due to the unavailability of circulating antibodies and lack of dendritic cells, microglia have a vital function in recognition of foreign material, phagocytosis and antigen presentation. However, microglia are not considered to be as effective APC as dendritic cells or macrophages [7]. MHC molecules are expressed by microglia, although at low levels, as they are actively down-regulated by the immune-quiescent microenvironment of the CNS. When activated, microglia demonstrate up-regulation of MHC molecules. However, to avoid excessive inflammation and tissue damage within the CNS, there is simultaneous activation of counter-regulatory mechanisms [8].
Microglia share many characteristics with macrophages—the main cell type of granulomatous inflammation. Fusing to giant cells they act to encapsulate the foreign body, separating it from normal tissues.
It is these unique immune features that allow retained surgical material to have such a delayed presentation in the CNS. As such a foreign body granuloma must be considered in the differential diagnosis of intracranial lesions in patients who have previously undergone surgery. Our case not only highlights this but also the continuing importance of adherence to the World Health Organization surgical checklist before closure.



