-
PDF
- Split View
-
Views
-
Cite
Cite
Ameer Kakaje, Mohammad Mahfouz, Hussain Chaban, Asymptomatic congenital intrapericardial diaphragmatic hernia in a woman becoming symptomatic after childbirth, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz281, https://doi.org/10.1093/jscr/rjz281
Close - Share Icon Share
Abstract
This paper describes a rare case presentation of congenital asymptomatic intrapericardial diaphragmatic hernia. In this case, the female patient survived without symptoms for over 30 years until becoming symptomatic at childbirth. Diaphragmatic hernia occurs when abdominal viscera protrude into the thoracic cavity, with pericardial hernias being the rarest type. Diaphragmatic hernia can be caused by trauma that raises the intra-abdominal pressure, whereas congenital hernias are often symptomatic at birth. It is rare to have a congenital asymptomatic intrapericardial diaphragmatic hernia, where the patient survives until adulthood and subsequently becomes symptomatic after delivering a child; hence, that is the uniqueness of this case.
INTRODUCTION
Congenital diaphragmatic hernia (CDH) occurs when abdominal viscera are permitted to herniate into the thoracic cavity through an anatomically defective diaphragm. CDH comes with high morbidity and mortality with an incidence of one in every 3000–4000 newborns [1, 2]. Congenital intrapericardial diaphragmatic hernia (IPDH) is the rarest form of CDH and is almost always symptomatic in early life. This paper reports a rare case, where congenital IPDH remained asymptomatic until adulthood. Very few similar cases have been reported in the literature to date.
CASE REPORT
A 35-year-old primigravida female patient complained of mild chest and epigastric pain. Twenty months earlier, she underwent a successful emergent caesarian surgery for preeclampsia, which was performed without complication. Since then, the patient complained of an episodic spasmo-colic pain in the left chest and abdomen that radiated to the left scapula and the upper back. On current presentation, she reported dyspnea and palpitation with sub-sternal heaviness. These symptoms were accompanied by a dry cough, orthopnea and palpitations. No change in bowel movements or any other complaints were reported or evident. She reported no history of surgery except for the cesarean section, which was uncomplicated. She reported no previous trauma, her family history was insignificant and the physical examination was normal. Pfannenstiel incision scar was well-healed with no erythema or drainage, and no tenderness or palpable masses were present around the scar or underneath it. Chest X-ray (Fig. 1) showed an enlarged cardiac silhouette, a closed left costo-diaphragmatic angle and an opacity that covered the left lower border of the heart and the left diaphragmatic dome. The right hemi-thorax was normal. Pleural effusion was suspected and thoracentesis was conducted. The drained fluid labs showed a neutrophilic exudative bloody liquid. Following this, a barium swallow (Fig. 2) was performed, which showed abdominal viscera to be herniated into the thoracic cavity with no other abnormalities. Chest and abdomen computed tomography (CT) scan with contrast (Fig. 3) showed a non-homogeneous opacity in the left side of the thoracic cavity that pushed the heart and other mediastinal components to the right. It was compatible with herniated abdominal viscera, suspected to be either a Morgagni hernia or as a result of a neglected trauma to the diaphragm (although the patient denied any trauma). Surgery was indicated using the thoracic approach. Under general anesthesia, the left chest was entered through the sixth intercostal space, and the thoracic cavity was found to be normal with no signs of hernia. The pericardium was opened and explored; the great omentum and colon were found to be protruded through the diaphragm into the pericardial sac. A defect of 5 cm in diameter was found in the central tendon of the diaphragm (Fig. 4). The adhesions between the pericardium, myocardium and the viscera were released. The viscera were then reduced back into the abdominal cavity through the hernia. The hernia was primarily sewed with running proline suture then covered with 5 × 5 cm proline patch which was supported with a pericardium patch. Finally, the pericardium was partially closed. Three days later, the chest drain tube was removed and the patient discharged in good status. A 2-week follow-up chest X-ray showed no abnormalities and monthly chest X-rays were indicated for a year, and were all normal.
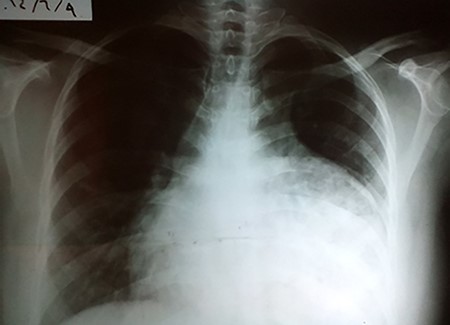
CXR showing an abnormal heart index and opacity that covers the left pleural angle.

Showing an abnormal barium swallow with viscera (red arrow) in the left hemi-thorax.
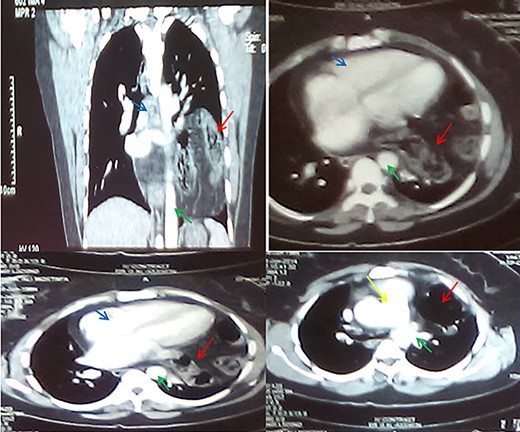
CT sections with contrast showing abdominal viscera in the thorax (red arrows), aorta (green arrow), the heart (blue arrows) and the pulmonary trunk (yellow arrow).
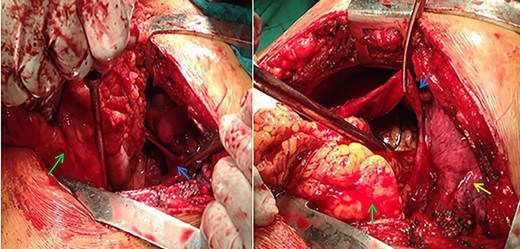
Real pictures in surgery shwoing the viscera (green arrows), the pericardium (blue arrows) and the lungs (yellow arrow).
DISCUSSION
CDH are frequently diagnosed early in life with the congenital IPDH being the rarest form. It is prominent by its symptoms in the respiratory and cardiac systems [3]. In IPDH, a defect lies in the diaphragm, causing an abnormal communication between the peritoneal and pericardial cavities. The diaphragm develops in the embryological period particularly during weeks 4–8. Early development errors cause a central tendon defect with Cantrell’s pentalogy that involved IPDH, and late errors will cause the possibility that IPDH will accompany pleuro-pericardial and peritoneo-pericardial defects and omphalocele [4]. Nevertheless, IPDH is the rarest of these anomalies, highly symptomatic in newborns, but variable when it presents in adulthood. It usually presents at birth or infancy with respiratory and cardiac symptoms with the other congenital defects described earlier [3]. IPDH symptoms are usually non-specific; patients can range from being asymptomatic to being symptomatic with fatal cardiac tamponade. IPDH usually presents with cardiorespiratory or gastrointestinal complaints. Time of presentation is usually variable depending on whether it is traumatic or congenital IPDH [5]. This could explain why the patient presented with chest and epigastric pain despite being asymptomatic for more than 30 years. We might speculate that her last pregnancy may have been the cause with her raised the intra-abdomen pressure creating the symptoms.
Minor traumatic events may be the cause of diaphragmatic hernias that may be overlooked by the patient in the cases of late-presented hernias. However, this cannot be confidently determined as the cause in most cases and we cannot rule out the possibility of a congenital etiology [4]. Many surgical approaches are available, such as transthoracic or a transabdominal, with laparoscopy and thoracoscopy, also indicated in particular cases. However, the thoracotomy approach was proposed in this case as adhesions were suspected in the chronically presented hernia, and the thoracic approach would provide better means to deal with these adhesions, through offering better visualization, and greater ease in detecting the hernia and reducing the viscera to the abdomen. Furthermore, a proline patch was indicated as the diaphragmatic defect was found to be large [6]. Proline patches can sometimes cause adhesions as they do not expand as do other options such as gortex. However, based on the surgeon’s experience, the view was taken that using a pericardium patch would minimize this particular risk of adhesions.
Asymptomatic congenital pericardial hernias, which become symptomatic after a certain even such as pregnancy, are rarely reported in the literature. The case reported here contributes unique information to the literature in this area.
References
Di



