-
PDF
- Split View
-
Views
-
Cite
Cite
Narendra Pandit, Tek Narayan Yadav, Deepa Shrestha, Purbesh Adhikari, Laligen Awale, IMFT of the sigmoid colon: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz334, https://doi.org/10.1093/jscr/rjz334
Close - Share Icon Share
Abstract
Inflammatory myofibroblastic tumor (IMFT) of the colon is a very rare entity, characterized by proliferation of myofibroblast cells admixed with inflammatory infiltrates. The entity was first described in the late 1990s, and since then less than 30 cases have been described. It frequently mimics other neoplasm of the colon, such as adenocarcinoma, lymphoma and stromal tumor, and is very difficult to clinch the diagnosis preoperatively based on the clinical and radiological findings. Here, we discuss an uncommon case of sigmoid IMFT in a 35-year old male, presenting with bleeding per rectum and managed successfully by colectomy.
INTRODUCTION
Inflammatory myofibroblastic tumor (IMFT) is a rare, nonmalignant tumor characterized by the proliferation of fibroblasts-myofibroblasts admixed with the plethora of inflammatory cells [1]. The tumor is commonly described for the lung; however, retroperitoneal and intrabdominal origin has been reported [2]. The first report from the colon was described in 1999; since then, less than 30 cases of colonic IMFT have been described in the English literature [1, 3]. The etiopathogenesis of the disease is unknown; however, it is thought to be the result of inflammatory response due to the infection, autoimmune dysregulation and surgery [4]. Here, we describe an uncommon case of colonic IMFT in a young male patient, presenting with blood mixed stool and mimicked colonic malignancy.
CASE REPORT
A 35-year-young gentleman presented to emergency department with 4-months history of blood mixed stool and fever (low-grade) for 1 week duration. He also complained of significant weight loss, anorexia and easy fatigability. On general physical examination, pallor was present, with localized tenderness in the left iliac fossa. His vitals were stable. Digital rectal examination revealed blood mixed stool without any intraluminal growth. The laboratory investigation revealed anemia (hemoglobin—7.6 g/dl), leucocytosis (total counts—14 600 cells/mm3) and normal liver and renal function tests. The serum carcinoembryonic antigen was within normal range. The contrast computed tomography (CT) abdomen and pelvis was done, which showed a large (8 × 5 cm), well-defined, homogenously enhancing intraluminal soft tissue lesion in the sigmoid colon, with few pericolic lymph nodes (Fig. 1). There were no features of intrabdominal metastases.
The diagnosis of bleeding malignant sigmoid colon tumor was made. The patient was further stabilized with transfusion of two pint of packed red blood cell and initiation of intravenous antibiotics in view of leucocytosis and localized tenderness, with suspicion of localized perforation. The patient then underwent emergency operation with Hartmann’s procedure. Intraoperatively, there was an intraluminal growth in the sigmoid colon, which was stuck to the lateral left pelvic wall, with a sealed perforation at the tumor site (Fig. 2). There were multiple pericolic lymph nodes, which were resected en bloc. The descending end colostomy with distal rectal stump closure was done. Postoperative period was uneventful and was discharged on postoperative day 7. The pathological report of the resected specimen showed proliferation of plump spindle cells arranged in singly scattered forms as well as in short fascicles. The cells were admixed with dense inflammatory cell infiltrates comprising plasma cells, lymphocytes, eosinophils and mast cells (Fig. 3). The section examined from the lymph node revealed lymphoid hyperplasia. The report confirmed inflammatory myofibroblastic tumor of the sigmoid colon. After 4 months, the patient underwent Hartmann’s reversal, and at 1-year of follow-up, the patient is fit and fine.
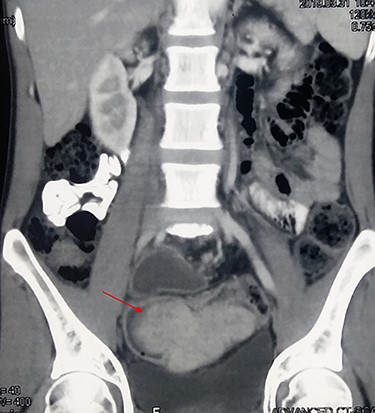
Contrast CT showing a large, enhancing, intraluminal soft tissue tumor (arrow) in the sigmoid colon.

Intraoperative (cut-open) specimen showing smooth, well-defined protruding intraluminal tumor with intact mucosa.
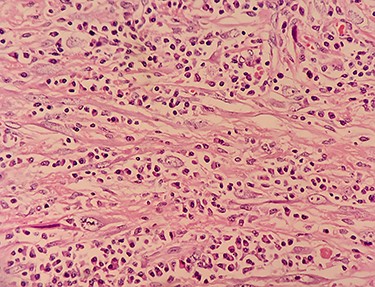
Photomicrograph (high power view; ·400) showing admixture of plasma cells, lymphocytes and spindle-shaped cells.
DISCUSSION
IMFT is a rare entity, which is commonly seen in the bronchial tree. The origin of this tumor from the extra-pulmonary site has been described, with few cases been reported from the colon [1, 4]. As the entity is rare, it is very difficult to pin-point the diagnosis based on the clinical and radiological examination. Here, we discuss the alarming signs to suggest the diagnosis and management of IMFT from the colon.
The tumor is commonly seen in children and young adults (median age 25 years) with no gender preference [5]. It is most commonly located in the distal and sigmoid colon; however, it can involve any segment of the colon and the rectum [1]. Although the tumor is benign in nature, the recurrence has been reported in few cases and hence listed by WHO as a tumor of undetermined malignant potential [2]. It has a nonspecific presentation such as bleeding per rectum, pain abdomen, loss of weight and appetite and rarely intestinal obstruction as described for the colorectal carcinoma [6, 7].
On contrast CT, the lesion does not have any specific features suggestive of IMFT. It can appear as ill-defined, nonencapsulated, protruding or infiltrative mass [8]. In the present case, it was large, intraluminal, well-defined, homogenously enhancing tumor mimicking lymphoma or gastrointestinal stromal tumor. The tumor in no way looked like a colonic carcinoma on imaging. On colonoscopy, the tumor appears as intraluminal soft tissue mass, with surface ulceration and intact mucosa. The biopsy usually reveals chronic inflammation [6]. In our patient, the colonoscopy was not done, as the tumor was bleeding with anemia, with probable localized perforation. Furthermore, the report would have not changed the management as the patient was planned for emergency surgery.
IMFT should be treated like a malignant colonic tumor, owing to its nonspecific clinical and radiological findings. The colonic resection with anastomosis/stoma should be done, depending on the site of the lesion and the mode of presentation [7, 9]. In a study by Gupta et al. [2], out of seven patients in their series, five required right hemicolectomy, one transverse and the remaining one underwent left hemicolectomy. Diagnosis is commonly made after surgery, with the pathological report characteristically showing spindle-shaped cells in bundles intermingled with inflammatory cells (plasma cells, eosinophils, neutrophils and lymphocytes). The cells invaded and ruptured the muscle layer, expanding through the submucosal [6]. Immunohistochemistry further confirms the finding by the positivity of PGM1, CD45 antigen, CD68, S100 and vimentin and negativity of desmin, smooth muscle actin, HMB-45, CD21, CD117 and pankeratin [10].
The prognosis of the disease after complete excision of the tumor is excellent, as the natural history of the tumor is benign. However, recurrence has been described in some cases, and hence long-term follow-up is recommended [1]. The role of chemotherapy, radiotherapy or nonsteroidal anti-inflammatory drugs is controversial with limited literatures; however, it may be considered for the unresectable, incompletely resected tumor or as a palliation, alone or in combination [2, 7].
In conclusion, IMFT is a rare entity in the colon with excellent prognosis. The differential diagnosis of it should be kept in mind in a young patient, with a well-defined intraluminal, enhancing soft tissue lesion in the colon.
Conflict of interest statement
None declared.
Disclosure
The authors have no potential conflicts of interest to reveal.



