-
PDF
- Split View
-
Views
-
Cite
Cite
Husain Esmaeil, Jamal Al-Fadhli, Abdullah Dashti, Nael Al-Sarraf, Ischemic mitral regurgitation in a patient with dextrocardia and situs inversus totalis, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz329, https://doi.org/10.1093/jscr/rjz329
Close - Share Icon Share
Abstract
Dextrocardia with situs inversus is a rare condition. Few previously published cases have addressed the observation of isolated coronary artery disease or isolated mitral valve disease in these patients. However, the occurrence of ischemic mitral regurgitation in such cases has never been previously reported. Here, we report such a case with emphasis on both surgical and echocardiographic features.
INTRODUCTION
Ischemic mitral regurgitation is rare in patients with dextrocardia and situs inversus (SI) totalis. Careful planning and adequate surgical set-up are important when dealing with such case. Transesophageal echocardiography (TEE) should be interpreted carefully using modification from the standard views to aid in understanding mitral valve.
CASE REPORT
A 57-year-old man known to have dextrocardia and SI totalis presented with anterolateral non-ST elevation myocardial infraction and pulmonary oedema. He had dyspnoea with New York Heart Association class III symptoms. His past medical history was significant for hypertension and type II diabetes mellitus. He was an ex-smoker for the past 2 years. There was no family history of heart disease. The apex beat was palpated on the right side, and a pan-systolic murmur was heard best at the apex. ECG showed depressed ST segment and T waves in leads V1-V6 (Fig. 1A). Chest radiography showed dextrocardia and cardiomegaly (Fig. 1B). Coronary angiography showed triple vessel disease (Fig. 1C and D). Transthoracic echocardiography revealed severe left ventricular dysfunction (ejection fraction 30%), severe global left ventricular hypokinesia and severe ischemic mitral regurgitation with eccentric jet directed anteriorly and tethered posterior mitral valve leaflet. He was stabilized medically and was referred for surgery.
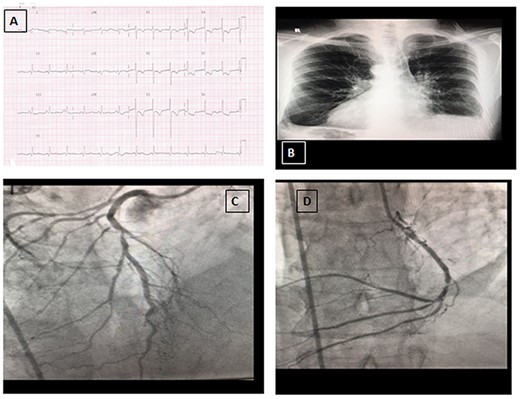
A: Electrocardiogram (ECG) on presentation. B: Chest radiograph showing dextrocardia. C: Coronary angiography view of left anterior descending artery (right sided). D: Coronary angiography view of circumflex artery (right sided).
He underwent Coronary Artery Bypass Graft (CABG) and mitral valve repair through a median sternotomy utilizing cardiopulmonary bypass (CPB) and cardioplegia cardiac arrest. Surgeon was standing on the left side of the patient. Great saphenous vein was harvested endoscopically from the left thigh and right internal mammary artery (RIMA) was harvested skeletonized. Ascending aortic cannulation and bi-caval cannulation were used. Cold-blood cardioplegia was administered antegrade in the aortic root. Aortic cross clamp was used. Systemic cooling to 32°C was used. Reversed great saphenous vein was anastomosed end-to-side to obtuse marginal branch of circumflex artery (performed with the surgeon standing to the right side of the patient), another reversed saphenous vein graft was anastomosed in a similar way to posterior descending artery, and RIMA was anastomosed to left anterior descending artery (both were performed with the surgeon standing on the left side of the patient). All distal anastomosis was performed first prior to mitral valve repair and prior to fashioning the proximal anastomosis on the ascending aorta. Mitral valve was approached through Sondergaard’s groove with surgeon standing on the left hand of the patient. The mitral valve showed tethering of p2/p3 segments. Down-size annuloplasty ring size 28 was used (Cosgrove-Edwards annuloplasty ring). After completion of proximal anastomosis, the clamp was removed, and patient was weaned off from CPB with inotropic support. Postoperatively, he developed junctional slow rhythm that required temporary pacing and then recovered. He also required inotropic support until third post-operative day. He was discharged to home on day 18 post-operatively. Pre-discharge echocardiography showed well-functioning mitral valve with no regurgitation. He was alive and well 6 months later.
DISCUSSION
Dextrocardia with SI affects 1:10 000 of population with incidence of coronary artery disease similar to the general population [1]. Previous cases reported isolated CABG in these patients using a variety of techniques [2]. These techniques ranged from conventional sternotomy to minimally invasive techniques [3]. Both off-pump and on-pump CABG were performed using arterial and venous conduits [4, 5]. A right-handed surgeon performed the surgery standing on the left side of the patient to have easier access to the surgical targets [5]. Other cases reported performing isolated mitral valve surgery in a similar population [6–9] both for rheumatic [6, 7] and degenerative mitral valve regurgitation [8, 9]. However, the performance of combined CABG and mitral repair in ischemic mitral regurgitation in patients with dextrocardia and SI totalis has not been reported. Approach to the mitral valve was conventionally by sternotomy [6–8] or by a thoracotomy [9]. Trans-septal approach to the mitral valve and the Sondergaard’s approach were both utilized with success.
TEE views in a patient with dextrocardia with SI are different than the standard views. In the midesophageal four-chamber view at 0°, the right atrium and the right ventricle are on the right side of the display (Fig. 2A). The midesophageal two-chamber view, usually obtained at a multiplane angle of 90°, is identical to the view seen in a patient with situs solitus (Fig. 2B). The midesophageal aortic valve long-axis view (LAX) was obtained at a multiplane angle of 30–40° (Fig. 2C), while the midesophageal aortic valve short-axis view (SAX) was obtained at a multiplane angle of 120–130° (Fig. 2D). The midesophageal Bicaval view was obtained at 76° (Fig. 2E). The transgastric mid-papillary SAX was obtained as expected at 0° but with the right ventricle on the right side of the display (Fig. 2F). So in summary, TEE views in dextrocardia patients are similar to situs solitus patients at a multiplane angle of 90°, they are mirror images of each other at 0°, while the aortic valve SAX and LAXs are “flipped” in comparison with situs solitus patients. The approach to mitral valve assessment with TEE must be altered [10]. Firstly, the multiplane angles required to assess different parts of the mitral valve leaflets are different. Secondly, when examining the valve using 2D TEE in the midesophageal aortic valve with LAX view in a dextrocardia patient, a leftward rotation of the TEE probe will examine the posterior portion of the valve (A3/P3) while in a situs solitus patient, such a leftward rotation would result in the anterior parts of the valve to be examined (A1/P1). This point is important when discussing mitral valve repairs or the position of paravalvular leaks. If the surgeon stands on the left side of the patient, then the surgical view of the mitral valve will be as shown in Fig. 3.
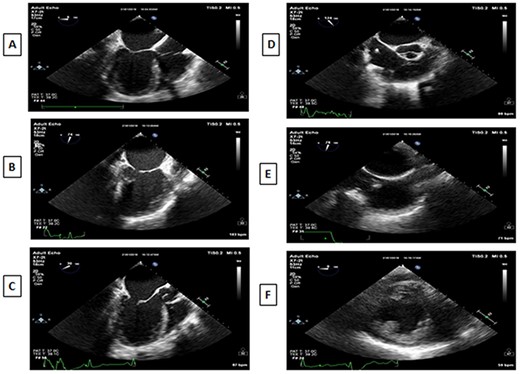
A: Midesophageal four-chamber view at 0°. B: Midesophageal two-chamber view at 90°. C: Midesophageal aortic valve LAX at 30°. D: Midesophageal aortic valve SAX at 120°. E: Midesophageal bicaval view. F: Transgastric midpapillary short axis view at 0°.
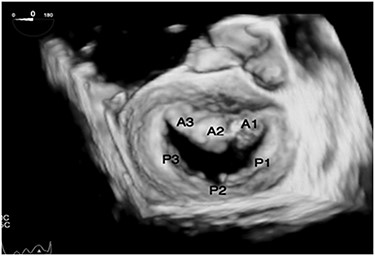
Transesophageal echo 3D view of mitral valve in dextrocardia as viewed intraoperatively by the surgeon standing on the left side of the patient.
CONCLUSION
Ischemic mitral regurgitation in patient with dextrocardia and SI totalis, conventional sternotomy and Sondergaard’s approach to mitral valve provided a good exposure and facilitated the operation with good outcome. Proper surgical exposure and planning with attention to TEE findings will aid in performing safe surgery for such cases.
Acknowledgement
None.
Funding
None.
Conflict of interest
None.



