-
PDF
- Split View
-
Views
-
Cite
Cite
Ralitsa Gencheva, Bryce Gibson, Shruthi Garugu, Anthony Forrest, Sumathilatha Sakthi-Velavan, A unilateral pelvic kidney with variant vasculature: clinical significance, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz333, https://doi.org/10.1093/jscr/rjz333
Close - Share Icon Share
Abstract
The incidence of ectopic pelvic kidney accounts for ~1 of 2500 live births. Although pelvic kidneys are most often asymptomatic, they may be associated with several pathologies including hypertension. As pelvic kidney results from a brief interference of the ascension of the developing kidney, it is frequently accompanied by an atypical and variable blood supply. The presence of multiple arteries and veins and their abnormal course and morphology are associated with surgical and radiological significance. Malrotation of the kidney with extrarenal calyces further predisposes the pelvic kidney to recurrent urinary tract infections. This report describes a rare case of a unilateral pelvic kidney with vascular and calyceal variations, and this case is reported to provide additional insight into this variation and its correlation to clinical practice.
INTRODUCTION
The kidneys are retroperitoneal organs surrounded by adipose tissue and located between the 12th thoracic vertebra and third lumbar vertebra. Pelvic ectopia accounts for 1 of 2500 births and is surgically and radiologically significant.
Pelvic kidneys are often asymptomatic and incidentally discovered. They are mostly supplied by the distal aorta, as is the case here, which is the vessel first and most severely affected by atherosclerosis, predisposing to segmental ischemia and hypertension [1]. However, the abnormal size of ectopic kidneys makes detection of ischemic events more difficult. Furthermore, because of the abnormal rotation, shape and vasculature, pelvic kidneys predispose patients to complications such as urinary tract infections (UTIs), renal calculi, uretero-pelvic junction obstructions, vesicoureteral reflux among many others. The abnormal kidney position also makes ectopic kidneys more vulnerable to physical damage [1]. This report describes a case of a cadaveric unilateral pelvic kidney with multiple vascular variations, extrarenal calyces and malrotation.
CASE REPORT
A unilateral pelvic kidney of abnormal morphology and vascular supply was discovered in a 65-year-old Caucasian male cadaver during dissection in the anatomy laboratory. The cause of death was Lewy body dementia. The intestines were removed, and the retroperitoneum was cleared of excess connective tissues. The left and right ureters were traced from renal pelvis to the urinary bladder. The renal vasculature was dissected bilaterally, and kidney dimensions were noted. The right kidney was located at L4–L5 vertebral level and was positioned anterior to the right psoas major with an anterior facing hilum, while the left kidney was located at T12–L3 vertebral level. The right kidney was smaller than the left and had an irregular shape and uneven surface (Tables 1–2). The arterial supply consisted of five arteries branching from a stem arising from the descending aorta, four of which entered the superior pole of the kidney and one entered the posterior surface. The abdominal aorta showed calcification suggestive of possible atherosclerosis. The pelvic kidney was drained by five renal veins, two of them emerged anteriorly and the rest emerged from the posterior aspect of the kidney. Four veins drained into the inferior vena cava, one of them drained into the left common iliac vein (Figs 1–4). All vasculature pierced through the capsule of the kidney instead of the hilum. Five major calyces emerged out of the hilum of the right kidney to converge into a single ureter. A sagittal cross-section of the pelvic kidney revealed malformed and abnormally located pyramids. The left kidney had normal morphology, and there were no major anatomical variations noted in the cardiac, respiratory, gastrointestinal and skeletal systems.
| Dimensions . | Right kidney . | Left kidney . |
|---|---|---|
| Length | 8.6 | 11.9 |
| Lower width | 5.2 | 5.0 |
| Middle width | 5.9 | 5.4 |
| Upper width | 3.3 | 5.7 |
| Ureter | 15.8 | 29.7 |
| Gonadal vein | 19 | 17.0 |
| Dimensions . | Right kidney . | Left kidney . |
|---|---|---|
| Length | 8.6 | 11.9 |
| Lower width | 5.2 | 5.0 |
| Middle width | 5.9 | 5.4 |
| Upper width | 3.3 | 5.7 |
| Ureter | 15.8 | 29.7 |
| Gonadal vein | 19 | 17.0 |
| Dimensions . | Right kidney . | Left kidney . |
|---|---|---|
| Length | 8.6 | 11.9 |
| Lower width | 5.2 | 5.0 |
| Middle width | 5.9 | 5.4 |
| Upper width | 3.3 | 5.7 |
| Ureter | 15.8 | 29.7 |
| Gonadal vein | 19 | 17.0 |
| Dimensions . | Right kidney . | Left kidney . |
|---|---|---|
| Length | 8.6 | 11.9 |
| Lower width | 5.2 | 5.0 |
| Middle width | 5.9 | 5.4 |
| Upper width | 3.3 | 5.7 |
| Ureter | 15.8 | 29.7 |
| Gonadal vein | 19 | 17.0 |
| Arteries . | Veins . | ||
|---|---|---|---|
| A1 | 5.3 | V1 | 10.3 |
| A2 | 2.5 | V2 | 5.3 |
| A3 | 1.8 | V3 | 2.5 |
| A4 | 1.5 | V4 | 3.7 |
| A5 | 2.9 | V5 | 8.4 |
| Arteries . | Veins . | ||
|---|---|---|---|
| A1 | 5.3 | V1 | 10.3 |
| A2 | 2.5 | V2 | 5.3 |
| A3 | 1.8 | V3 | 2.5 |
| A4 | 1.5 | V4 | 3.7 |
| A5 | 2.9 | V5 | 8.4 |
| Arteries . | Veins . | ||
|---|---|---|---|
| A1 | 5.3 | V1 | 10.3 |
| A2 | 2.5 | V2 | 5.3 |
| A3 | 1.8 | V3 | 2.5 |
| A4 | 1.5 | V4 | 3.7 |
| A5 | 2.9 | V5 | 8.4 |
| Arteries . | Veins . | ||
|---|---|---|---|
| A1 | 5.3 | V1 | 10.3 |
| A2 | 2.5 | V2 | 5.3 |
| A3 | 1.8 | V3 | 2.5 |
| A4 | 1.5 | V4 | 3.7 |
| A5 | 2.9 | V5 | 8.4 |

Posterior abdominal wall and pelvis. 1. Right (Pelvic) kidney, 2. inferior vena cava, 3. thoracic aorta, 4. left kidney, 5. ureter, 6. liver, 7. urinary bladder, 8. renal vein, 9. renal artery, 10. gonadal vein, 11. common iliac artery, 12. common iliac vein, 13. external iliac artery, 14. psoas major, 15. iliacus, 16. rectum, 17. gall bladder.
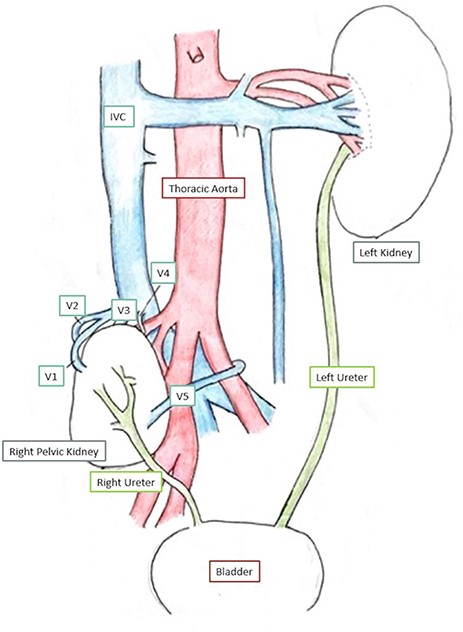
Schematic diagram of kidneys and vasculature. V1–V5—renal veins.
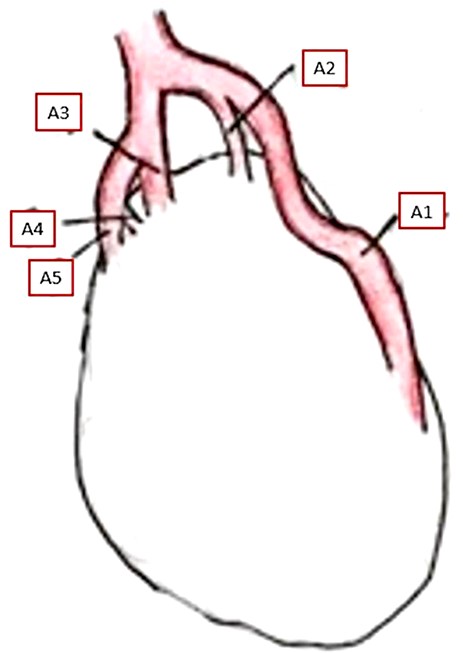
Posterior aspect of the pelvic kidney showing its arterial supply. A1–A5—renal arteries.
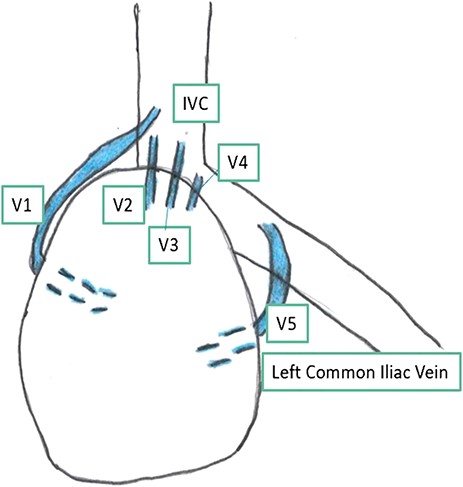
Posterior aspect of the pelvic kidney showing its venous drainage. V1–V5—renal veins.
DISCUSSION
Kidney development proceeds between the sixth and eighth weeks of life with kidney ascent occurring during the ninth week. Renal ectopia occurs due to brief interference of kidney ascension by the failure of degeneration of fetal renal blood supply or lack of factors responsible for ureteral growth and elongation [2, 3]. Multiple renal arteries are the most common variant among ectopic cases, with an incidence rate of 20–30%. Considering the increase of renal transplants and the use of laparoscopic techniques, detailed knowledge of ectopic kidneys is essential [4, 5]. Laparoscopic techniques employ a limited surgical window, thus making variant vasculature a potential obstacle to successful surgery especially if there is a lack of detailed knowledge of the variant vasculature. Presurgical computed tomography angiography is suggested as a way to circumnavigate difficult surgical cases [5]. Furthermore, multiple renal arteries have been linked to elevated plasma renin levels and an increased likelihood of hypertension [6]. The calcified aorta noted here substantiates the correlation between an increased likelihood of hypertension in patients with renal ectopia. Furthermore, due to the size difference between both kidneys in this donor, the pelvic kidney may have decreased functional capacity if any at all. This case has a unique vasculature which has not been reported before, with multiple arteries entering the kidney, a prehilar branching pattern, which is clinically significant and can easily be identified in 3D imaging [1, 5]. The vasculature of the pelvic kidney has been reported as complicated and highly variable, due to retention of its fetal blood supply. The arterial supply can arise from several sources including the aorta, common iliac artery, external iliac artery and internal iliac artery. Knowledge of these anatomical variations is beneficial for patients undergoing abdominal surgery with pelvic kidneys [7]. Any anomaly in the renal arteries’ origins can stop the ascension and cause ectopia or rotation anomalies, and this could explain malrotation in this case [4]. Multiple renal veins are also seen in patients with ectopic kidneys, with an incidence rate of 15–30%, similar to that of arterial variance [5]. In this case, there is a renal vein which crossed the midline which presents an increased risk of injury to vessels or the kidney itself during abdominopelvic surgical procedures.
Another variation seen in this case is the extrarenal calyces. This type of abnormality is one of the rarest occurrences associated with renal ectopia, with only 20 cases reported this far. Although the cause of extrarenal calyces has not yet been determined, it has been speculated to occur because of difference in the speed of development between the metanephric mass and ureteric bud [8]. Extrarenal calyces predispose patients to recurrent UTIs or obstructions, both of which may cause long-term renal damage and must be monitored for in patients with known anomalies similar to this case [3].
Although pelvic ectopic kidneys are often found incidentally, they can be associated with complications such as urolithiasis, hydronephrosis, renal calyces, ureteropelvic junction obstruction, hypertension and renal carcinoma [1, 3, 7, 8]. One in ten thousand individuals who have renal abnormalities also present with vertebral, cardiac and limb defects, anal atresia and trachea-esophageal fistulas, none of which were discovered in this case [9]. The clinicians should be aware of the possible surgical complications and clinical presentations in patients with pelvic kidney and exercise caution to avoid inadvertent damage to the variant vasculature during surgery.
Conflict of Interest statement
The authors declare there are no potential conflicts of interest.
Funding
This work was supported by Marian University College of Osteopathic Medicine.
Ethical Approval
The research was conducted on a cadaver, and the materials do not contain personal identifiers. The Institutional Review Board of Marian University reviewed the protocol and determined the study as appropriate for exemption under federal regulations.
Consent
Not applicable.
Guarantor
Guarantor for the article is ‘Sumathilatha Sakthi Velavan’.
ACKNOWLEDGEMENTS
The authors are grateful to the donor who donated his body to the medical school involved in this research and to his family and friends. We would like to thank Marian University College of Osteopathic Medicine, Division of Biomedical Sciences for allowing us to collect data from the cadaver and supporting this research.



