-
PDF
- Split View
-
Views
-
Cite
Cite
William T McSweeney, Brian Kirkby, Combustion of pneumoperitoneum: a rare danger in the operating room, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz323, https://doi.org/10.1093/jscr/rjz323
Close - Share Icon Share
Abstract
Fire or combustion occurring during laparotomy is an uncommon and potentially hazardous event that can be precipitated by the use of surgical energy devices in the presence of enteric gases or exogenous materials present in the abdomen such as alcohol. Oxygen necessary for a combustive event can be increased in the setting of a proximal enteric injury and with higher concentrations of inspired oxygen during anaesthesia. We report on a case of combustion on entry to the abdomen using monopolar diathermy during exploratory laparotomy for gastric antral perforation in the presence of alcohol and enteric gases.
INTRODUCTION
Operating room fire events are thankfully rare occurrences, usually relating to a well-established ‘fire triad’, composed of an oxidizer, fuel and an ignition source [1]. The most commonly implicated surgical specialty is head and neck surgery, followed by facial surgery, and the most commonly involved ignition source is the handheld diathermy [2]. Oxygen and nitrous oxide are common oxidizers present during such an event, while surgical drapes and gastrointestinal gases can serve as fuels [3]. When considering risk reduction principles relating to operating room fires or combustive events, it is important to understand that certain factors such as proximal enteric perforation, artificially oxygen-enriched environments created by draping or even the presence or absence of bowel obstruction can confer a higher risk of these events in the surgical environment [3].
CASE PRESENTATION
We report a 35-year-old male who presented to the emergency department with severe epigastric pain, nausea and vomiting. He had no prior history of gastro-oesophageal reflux disease or trauma and denied any medical comorbidities. He had a virgin abdomen surgically. He was a current smoker (15 cigarettes per day) and sporadic binge drinker, with last alcohol consumption reportedly 1 day prior of uncertain quantity. He denied any non-steroidal anti-inflammatory drug use, history of peptic ulcer disease, or previous gastroscopy. He took no regular medications.
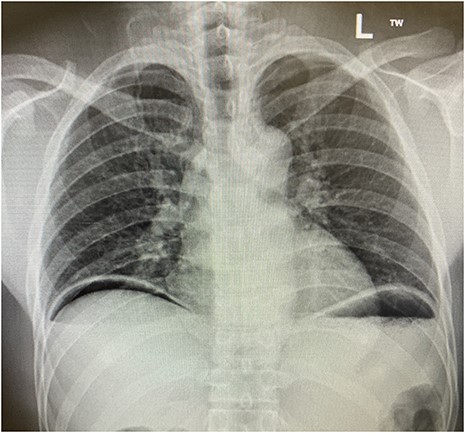
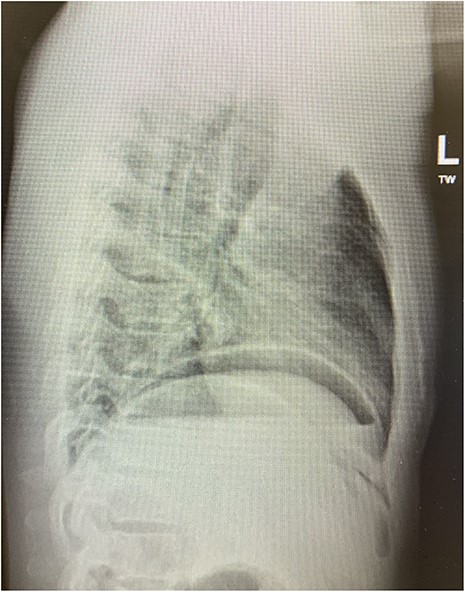
On examination in the emergency department, he was found to have localized peritonism to the epigastrium and was diaphoretic. An urgent erect chest radiograph (Figs 1 and 2) was revealing of gross pneumoperitoneum, presumably of a hollow viscous perforation as the source. General surgery was consulted after the presence of free air was detected. In the setting of the patient’s virgin abdomen and unremarkable surgical history, with peritonism and free intraperitoneal gas, the patient proceeded directly to urgent exploratory laparotomy with concurrent resuscitation measures, including intravenous fluid resuscitation and placement of an indwelling catheter.
The patient proceeded to be pre-oxygenated in the operating theatre with 100% oxygen via bag-valve mask, before a rapid sequence induction and conventional preparation of the abdomen with aqueous Betadine and draping with square surgical drapes. Upper midline laparotomy approach was decided upon, and incision through the skin and subcutaneous tissues was initiated with a size 15 scalpel blade and continued with monopolar diathermy until the peritoneum was encountered. Upon attempting to enter the peritoneum, which was tense and distended, a loud ‘pop’ was heard, with a sudden rush of air and heat generated at the end of the diathermy. There were no obvious injuries to the patient from this combustion event or to the surgical team and laparotomy proceeded. A localized 1 cm perforation of the antrum of the stomach was found with contamination of enteric contents locally. An omental patch repair was performed with 3-0 Prolene sutures to plicate omentum over the defect before a wash of the abdomen with warmed saline and placement of a 15-French Blake’s drain and closure of the abdominal wall.
The patient was transferred to the surgical ward for ongoing cares, remaining nil by mouth and commenced on intravenous antibiotics and proton pump inhibitor infusion. On post-operative day 3, a follow-through contrast study showed no leak of enteric contents from the stomach (Fig. 3) with transit of the contrast into the duodenum, and a concurrent ileus was shown with prominent small bowel loops (Fig. 4). A clear fluid diet was initiated, with gradual upgrade before discharge to usual residence and follow-up gastroscopy as outpatient.


DISCUSSION
The occurrence of a combustive event during surgery has been rarely reported on, but remains a serious potential complication with significant morbidity. The aetiology of fire in the operating room relates to the well-established ‘fire triad’, endorsed by the American Society of Anesthesiologists [1]. This triad includes an oxidizer, an ignition source and fuel. Specific to the operating room, commonly present oxidizers include oxygen and nitrous oxide. Importantly, the local concentration of oxygen can be enriched when the configuration of drapes and open oxygen sources promote pooling of an oxygen-enriched atmosphere. Ignition sources in operating room fires include electrocautery devices, drills, argon beam coagulators or even defibrillator pads. Finally, fuel sources can include surgical drapes and alcohol-containing preparation solutions, as well as gastrointestinal tract gases or even exogenous alcohols [1].
Bellevue et al. [4] reported a case report of fire in the operating theatre in the setting of perforated viscous and laparotomy, with a self-extinguishing blue flame erupting from the peritoneal cavity. Similarly, Thomas and Wilson [5] described a spontaneous combustion of the gas-filled peritoneum in the setting of proximal small bowel perforation. They concur that electro-surgery devices are the most common energy source for ignition. Importantly, when considering the presence of an oxidizer, the consideration of anaesthetic pre-oxygenation is paramount. The concentration of oxygen in the gastrointestinal lumen decreases distally but is artificially increased in this setting. When reviewing the fire triad, it is pertinent to understand that a proximal enteric perforation will expose the peritoneum, and therefore the ignition source upon entry to this space, to a higher concentration of oxygen. This can be artificially enhanced by anaesthetic techniques [5]. Historically, other sources of an oxidizer included peritoneal insufflation with oxygen or nitrous oxide; however, the newer use of carbon dioxide confers the advantage of higher blood solubility and has an inhibitory effect on flammability [3].
When considering sources of fuels in the fire triad, such as gastrointestinal gases or surgical drapes, it is important to understand the presence of specific fuels during altered metabolic states or differing patient populations. Hydrogen and methane are the most common fuels of the gastrointestinal tract that may serve as a flammable source, but these can be reduced by certain states such as low residue diet, fasting or adequate bowel preparation [3]. Inversely, the concentration of combustible gas can be increased by preparation of the colon pre-operatively with mannitol or lactulose [5]. Importantly, despite the explosive range of hydrogen and methane, neither is combustible in less than 5% oxygen, a concentration that is easily achieved in the proximal gastrointestinal tract with approximately 10% being present in the stomach reducing distally. Additionally, this will be further increased during anaesthesia utilizing oxygen [3]. This hypothesized mechanism is supported in a report by Dhebri and Afify [3]. They describe an explosion during emergency laparotomy for perforated bowel, which was confounded by cardiopulmonary resuscitation pre-operatively, which likely increased gaseous distention of the stomach and the availability of fuel.
Lastly, when considering ignition sources, a recent review suggests that diathermy is the most common ignition source [6]. However, the most common site of fire is during tonsillar surgery, with facial surgery being the second most common [2]. Interestingly, it appears that handheld diathermy has been reported in the literature as a source during times of obstruction, poor bowel preparation or preparation with mannitol [7–9]. Some authors recommend against the use of diathermy for entry into the gastrointestinal lumen for this reason [7, 8]. Other ignition sources such as argon beam coagulators or even defibrillator pads can also be implicated.
This report of a rare combustive event on entry to the peritoneum during a proximal enteric perforation highlights numerous elements of the fire triad. The presence of a proximal perforation exposes the peritoneum and the handheld diathermy to a higher concentration of oxygen, which is further increased by anaesthetic pre-oxygenation. The presence of alcohol having been previously consumed may also have had a contributory effect on combustion. In addition, the concentration of oxygen required for gastrointestinal gases to be combustible is more readily achievable at this proximal level of the gastrointestinal tract. Overall, this case represents an example of numerous contributing factors of the fire triad being present and in ideal conditions to predispose to a combustive event.
AUTHOR CONTRIBUTIONS
W.T.M. contributed to the conception and design of the study. B.K. contributed in a supervisor role. All authors read and approved the final version of the manuscript.
Conflict of interest statement
None declared.
Funding
None.
Ethical approval
An informed consent was obtained from the patient.



