-
PDF
- Split View
-
Views
-
Cite
Cite
Yujiro Yokoyama, Masato Nakajima, Intrapericardial rupture of distal aortic arch aneurysm, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz343, https://doi.org/10.1093/jscr/rjz343
Close - Share Icon Share
Abstract
Intrapericardial rupture of an aortic arch aneurysm is a rare and catastrophic event that requires emergency treatment. Recent development of thoracic endovascular repair has contributed to improved outcomes for the treatment of ruptured aneurysm of the thoracic aorta. However, when there is an aneurysm that involves the arch vessels, the treatment strategy, including conventional open surgery and endovascular stenting, is still controversial. We performed life-saving emergency total arch replacement using a modified elephant-trunk procedure for two cases of intrapericardial rupture of an aortic arch aneurysm. Prompt institution of cardiopulmonary bypass is effective for reducing the risk of re-rupture. Hybrid operation caries the risk of re-rupture during the procedure because it is performed under heparinization without blood pressure control. Open surgery is still a good option for such cases.
INTRODUCTION
Intrapericardial rupture of an aortic arch aneurysm is uncommon but recognized as a catastrophic event with an extremely high mortality rate. Recent development of thoracic endovascular repair has contributed to improved outcomes for the treatment of ruptured aneurysm of the thoracic aorta. However, when there is an aneurysm that involves the arch vessels, the treatment strategy including conventional open surgery and endovascular stenting is still controversial. In this report, we describe two surgical cases of ruptured aortic arch aneurysm complicated with hemodynamic shock due to cardiac tamponade. Prompt diagnosis and emergency conventional open surgical repair have several benefits and still remain an effective method despite recent advances in endovascular treatment.
CLINICAL REPORT
Case 1
An 82-year-old man was brought to the emergency department in our hospital with loss of consciousness. Although he was alert and conscious, his blood pressure was 90/40 mmHg, his heart rate was 100 bpm and he had an agonized look with pain. Transthoracic echocardiography revealed the presence of fluid in the pericardium (Fig. 1). Contrast-enhanced computerized tomography showed an aortic arch aneurysm and pericardial effusion, so we decided to perform an emergent operation based on the diagnosis of intrapericardial rupture of an aortic arch aneurysm. After median sternotomy, there was abundant pericardial effusion with coagulation and foramen lacerum at the lesser curvature penetrating into the pericardium. Cardiopulmonary bypass (CPB) was established immediately after sternotomy via the ascending aorta and right atrium. When the rectal temperature reached 26°C, circulatory arrest was initiated. During the period of arrest, antegrade cerebral perfusion was performed. For myocardial protection, blood cardioplegic solution was infused intermittently through the antegrade cannula. We conducted a total aortic replacement with a modified elephant-trunk procedure using a 22 × 10 × 8 × 8-mm Intergard 4-branch graft. The CPB time, aortic clamp time and total circulatory arrest times were 184, 94 and 58 minutes, respectively. The patient recovered well and was discharged from the hospital without complications. The patient was contacted by telephone and was alive without complications at 57 months.
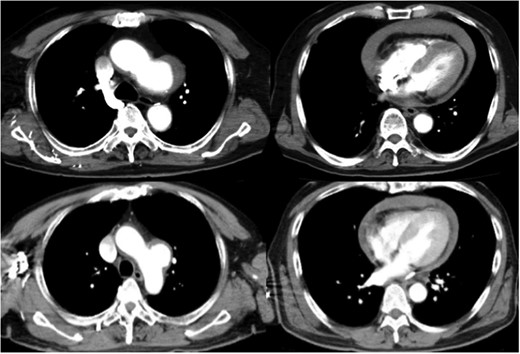
Preoperative computed tomography shows a distal arch aneurysm and pericardial effusion (top: Case 1; bottom: Case 2).
Case 2
A 58-year-old man came to the emergency department in our hospital because of the sudden onset of severe back pain. He was alert, his blood pressure was 93/70 mmHg and his heart rate was 102 bpm. Transthoracic echocardiography revealed pericardial effusion. Pericardiocentesis was performed, and it showed bloody fluid. Contrast-enhanced computed tomography showed a distal aortic arch aneurysm and pericardial effusion (Fig. 1), so the diagnosis was intrapericardial rupture of an aortic arch aneurysm, and emergent surgery was performed. At the operation, the heart was covered with coagulation, and we found the foramen lacerum at the aneurysm that penetrated the precardium (Fig. 2). We performed total arch replacement using the same method as described in the first case. The CPB time, aortic clamp time and total circulatory arrest times were 177, 83 and 56 minutes, respectively. The patient recovered well and discharged from the hospital without complication. He was alive and had no complications at 26 months, the time of his last appointment.
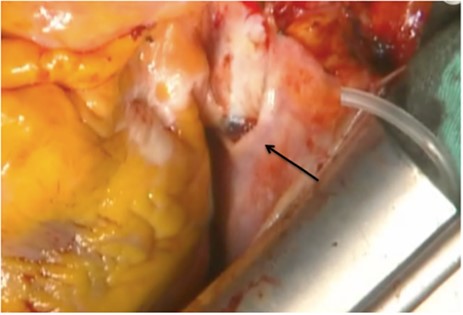
The foramen lacerum at the aneurysm that penetrates the pericardium (arrow).
DISCUSSION
Ruptured thoracic aortic aneurysm (TAA) is a rare and catastrophic event that requires emergency treatment [1]. Johanson et al. reported that more than 50% of the patients with ruptured TAA died within 6 hours, and only 41% of the patients were alive on arrival at the hospital [2]. TAA usually ruptures into the thorax, mediastinum and lung; however, intrapericardial rupture is extremely rare.
The management of TAA with intrapericardial rupture is different from typical TAA rupture because of hemodynamic instability due to cardiac tamponade. Immediate diagnosis using contrast-enhanced computed tomography and immediate resolution of tamponade are important. However, the risk of re-rupture still remains even after the hemodynamics is stabilized. One of the key factors for reducing the risk of re-rupture is the prompt institution of CPB, as described by Kim et al [3]. We performed surgical repairs in two cases of intrapericardial rupture of TAA, and CPB was initiated immediately after sternotomy, thereby preventing re-rupture. Several surgeons reported that a hybrid operation, the arch-debranching procedure, can serve as an alternative to open surgery [4,5]. However, it carries the risk of re-rupture during the procedure, because it is performed under heparinization without blood pressure control. A hybrid operation that combines open repair and endovascular stenting could be an effective alternative in cases where distal reconstruction of an arch aneurysm is technically difficult [3].
Conclusion
Intrapericardial rupture of TAA is rare and requires emergency treatment. Open surgery is still the gold-standard treatment, because it has been proven to be effective and rapidly reduces the risk of re-rupture.
Conflict of interest statement
None declared.



