-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Rogers, Hong Lee, Kedar Jape, Zi Qin Ng, David Koong, Vaginal evisceration of small bowel, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz317, https://doi.org/10.1093/jscr/rjz317
Close - Share Icon Share
Abstract
Evisceration of bowel through the vaginal vault is an extremely rare condition and is considered to be a surgical emergency. We present the case of an 83-year-old female who was brought to the emergency department with a vaginal prolapse complicated by evisceration of small bowel. A midline laparotomy was performed for reduction of the bowel with a subsequent vaginal repair. We present this case due to its rarity and high-reported mortality rate.
INTRODUCTION
We present the case of an 83-year-old female who was brought to the emergency department with evisceration of small bowel through a ruptured vagina. Midline laparotomy was performed for reduction of small bowel with associated vaginal repair.
CASE REPORT
An 83-year-old female presented with evisceration of small bowel through a perforated vaginal vault. The day of ED presentation, the patient was straining in an attempt to pass stool due to her severe constipation. During this period of straining, she experienced sudden onset of pelvic pain and noticed evisceration of small bowel through her perineum.
Her medical history is notable for hypertension, prior abdominal hysterectomy years in the past and vaginal prolapse managed conservatively with oestrogen pessaries.
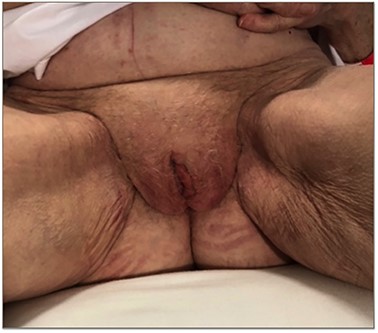
On arrival to the emergency department, her vital signs were within normal limits despite being in significant distress. Examination demonstrated a soft, non-tender abdomen with a Pfannenstiel scar. On examination of the perineum, there was evisceration of ~200 cm of small bowel with mesentery through a perforated prolapsed vaginal vault. The small bowel appeared mildly congested and ischaemic (Fig. 1). Anal and rectal examination was normal.
She was kept nil by mouth and commenced on intravenous hydration. Broad-spectrum intravenous antibiotics (Ceftriaxone 1 g and Metronidazole 500 mg) were administered. A large sterile pack soaked with warm saline was used to wrap around the small bowel loops. Initial attempts at vaginal reduction were unsuccessful. She was promptly taken to theatre by the General Surgical team, with assistance from the Gynaecology team. The patient was placed in a modified LLoyd-Davies position and a lower midline laparotomy was performed. The small bowel was reduced trans-abdominally with gentle manipulation through the perforated vaginal vault. The perforated vaginal vault appeared necrotic around the edge, with prominent ulceration seen at the proximal end of the vaginal wall. With the benefit of adequate access via an open approach, the anatomical relation between the rectum and bladder from the vault were clearly defined. The entire length of small bowel was inspected and appeared viable. The Gyneacology team using interrupted 2/0 Vicryl sutures repaired the perforated vaginal vault. Debridement of the necrotic vaginal edge was also performed to optimize healing. Copious amount of warm saline wash was used and a vaginal pack was left in situ for support. The time from symptom onset to laparotomy was calculated at ~4 hours.
Definitive management of vault prolapse like colpocleisis, sacrospinous fixation and sacrocolpoplexy were not performed in the context of an emergency surgery.
She was initially managed under the Gynaecology team in the High Dependency Unit with daily vaginal packing and application of topical oestrogen for 2 weeks.
Upon multidisciplinary discussion, given continued voiding and stool passage difficulty with ongoing prolapse, an elective LeFort colpocleisis was planned. In preparation for this procedure, examination revealed a stage three cystocele, rectocele and vault prolapse with inverted vaginal vault due to the recent suturing at emergency surgery (Fig. 2). Small decubitus ulcers were also noted despite oestrogen usage. The procedure involved denudation of the rectangular portion of mid anterior and posterior vaginal walls followed by plication of pubocervicovesical and rectovaginal fascia. A posterior colpoperineorrhaphy and levator ani plication were performed at the same time. (Fig. 3).

Vaginal evisceration of small bowel through prolapsed vagina on initial presentation to ED

Post-operative image with small bowel reduced but remaining vaginal prolapse
The patient recovered well from the colpocleisis and is awaiting followup in outpatient clinic.
DISCUSSION
Pelvic organ prolapse affects 40% of the female population according to the Women’s Health Initiative trial. Understanding of normal vaginal support is essential to provide appropriate management for specific types of prolapse. Delancey has described vaginal support in three levels. Level one occurs at the apex of the vagina with the support provided by the uterosacral–cardinal complex. Level two is when the arcus tendinous fascia pelvis (anterior vagina) and arcus tendineus levator ani (posterior vagina) provides support to the middle part of the vagina. Level three support is provided by the urogenital diaphragm and perineal body to the distal part of vagina [1]. In our case, through having all three levels of prolapse, it was the apical support deficiency that led to complete vaginal eversion. This eversion, compounded by atrophic vaginal epithelium resulted in evisceration of bowel.
Evisceration of bowel through the vaginal vault is a rare condition and is considered a surgical emergency. A literature review by Nasr et al. [2] from 1900 to 2004 concluded that <100 cases had ever been reported. In a review of 12 patients by Croak et al., patients usually present with pain, vaginal bleeding and abdominal pressure [3].
Vaginal evisceration most commonly effects menopausal women, those who have had a hysterectomy or those with previous vaginal surgery. In those who are premenopausal, coital trauma, instrumentation or obstetric injury is the predisposing factor [2]. Croak et al. reports a mean age for evisceration of 62 [3].
Given a reported mortality rate of 6%, evisceration of small bowel through the vagina is a surgical emergency [4]. Complications associated with this condition include ischaemia, abdominal sepsis and deep vein thrombosis (DVT) [5,6]. There are multiple surgical techniques, which have been employed for treatment of this condition including transvaginal, laparotomy, laparoscopic and mixed [7].
Decisions on course of management should be based on patient factors, most importantly on the viability of bowel. In our case, we opted for laparotomy given initial evaluation of the bowel identified the possibility of ischaemia. In cases where the bowel seems viable, transvaginal approaches should be considered. Matthews and Kenton [8] report four successful transvaginal repairs of bowel evisceration in the setting of no peritonitis or bowel injury.
We present this case to raise awareness of management strategies given the significant mortality rates associated with this condition. Secondly, it emphasizes the importance of interdisciplinary surgical cooperation to achieve the best possible outcome for patients.
DECLARATION
The corresponding author has received no research scholarship. This submission has not been concurrently communicated with any other journal or association



