-
PDF
- Split View
-
Views
-
Cite
Cite
Ashraf Alshabatat, Shaden Srayrah, Sameer Aljfoot, Laith Obiedat, Sakher Alsharoa, Kristi Janho, Omar Alzoob’I, Endovascular treatment of iatrogenic iliocaval fistula post lumbar disc surgery, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz313, https://doi.org/10.1093/jscr/rjz313
Close - Share Icon Share
Abstract
A 39-year-old patient presented with a history of right-side heart failure (dyspnea and orthopnea), right lower extremity deep vein thrombosis, and hepatic impairment. A physical exam showed increased jugular venous pressure, hepatomegaly, and bilateral lower limb pitting edema. A computed tomography angiograph revealed an arteriovenous communication between the right iliac artery and inferior vena cava (IVC) at the level of L4/L5. The patient was diagnosed with a large arteriovenous fistula (AVF), which developed post lumbar disc surgery. Fistulas between the common iliac arteries and IVC are very rare post lumbar disc surgery. Acquired iliocaval AVF is much more difficult to treat surgically because of the risk of massive hemorrhage. The patient underwent a successful endovascular stent graft repair. The patient’s symptoms of heart failure including exertional dyspnea and orthopnea were resolved 6 months post surgery.
INTRODUCTION
Arteriovenous fistulous communication between the inferior vena cava (IVC) and the common iliac arteries (iliocaval fistula) is extremely rare (approximately < 1%) compared with fistulous communication between the aorta and the IVC [1]. The increase in the number of interventional procedures (both vascular and nonvascular) performed over the last decades has resulted in an increase in complication from iatrogenic arteriovenous fistulas (AVFs). Vascular injury after posterior surgery to the lumbar spine is very rare, with an incidence of approximately 1–5 in 10 000 [2].
The mean time for the diagnosis of an AVF varies from months to years; there have been reports of the discovery of an AVF up to 11 years post lumbar discectomy operation [3]. Often, this diagnosis is missed because of the rarity of iliocaval fistula and the vague nature of complaints.
In patients with large AVFs, the increase in venous return results in cardiomegaly. If left untreated, cardiac decompensation ensues, and the patient manifests the symptoms and signs of high-output congestive heart failure, including lower extremity swelling, venous congestion involving the liver, dyspnea, and hypotension.
We report a case of successful treatment of high-output heart failure by endovascular intervention, which was caused by iliocaval fistula that developed post lumbar disc surgery. Hospital ethical committee approval was obtained.
CASE REPORT
A 39-year-old male patient was transferred to our center with a history of right-side heart failure (dyspnea and orthopnea), right lower limb deep vein thrombosis (DVT), and hepatic impairment. The only relevant medical event in the medical history of the patient was herniated lumbar disc surgery 6 years earlier. The patient was on heart failure medication.
A physical examination showed hepatomegaly, bilateral lower limb pitting edema (more on the right side), a continuous bruit in the lower abdomen, and increased jugular venous pressure. A cardiac echocardiography showed elevated pulmonary artery pressure, normal left ventricle systolic function, and an enlarged right ventricle. A venous duplex showed DVT in the right femoral and popliteal veins. Computed tomography angiography (Fig. 1) with 3D reconstruction revealed an arteriovenous communication between the right iliac artery and the IVC at the level of L4/L5, which was the site of the previous disc surgery, as well as a dilated IVC with a diameter of 7 cm.
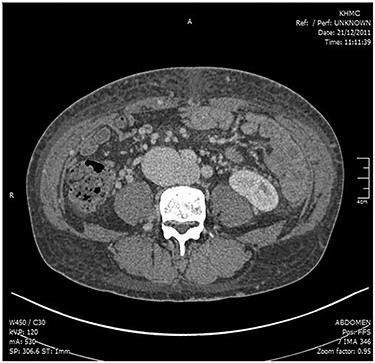
CT angiogram showing the connection between the right iliac artery and the IVC.
The patient underwent an endovascular repair of his AVF under spinal anesthesia. An Endurant (Medtronic, Inc., Minneapolis, MN) iliac stent graft was successfully deployed (Fig. 2). The patient had an IVC with a large diameter and low venous inflow owing to right lower limb DVT. Therefore, we decided to create an AVF at the groin with a limited inflow (200–300 mL/minute) between the common femoral vein and femoral artery using a tapered expanded polytetrafluoroethylene graft. The graft was closed after 3 months.
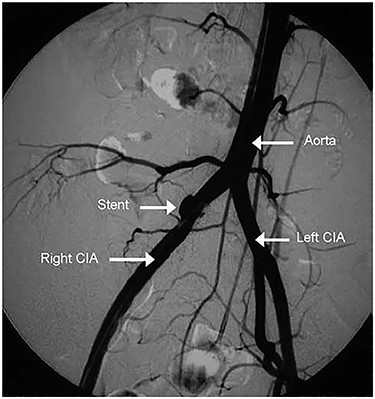
Post stent graft deployment angiogram showing the stent in position and the disappearance of AVF.
The patient’s symptoms of heart failure including exertional dyspnea and orthopnea were resolved after 6 months. A follow-up Doppler ultrasound confirmed the anatomic correction, and a resolution of the dilated heart chambers, a decrease in the diameter of the IVC to 4 cm, and a decrease in pulmonary pressures were confirmed with an echocardiogram. At the present time, 4 years postoperatively, the patient is doing well.
DISCUSSION
In patients with large AVFs, the increase in venous return results in cardiomegaly, which can acutely develop within weeks or months of the injury or progressively increase in severity over a period of years. Our patient developed symptoms and signs of heart failure a few months after surgery, but unfortunately the underlying cause was only discovered after 6 years.
An AVF can form immediately post lumbar surgery if the laceration includes both arterial and venous tears. An arterial hemorrhage evacuates through the venous defect, leading to small bleeding or retroperitoneal hematoma [4]. The patient does not develop hypotension because of the absence of extravasations. The fistula can appear months or years later [3]. The flow in the artery proximal to the fistula can increase up to 5-fold if the fistula is 1.5 times larger than the arterial diameter and 8-fold if the opening is 3 times larger than the inflow artery [5]. As the flow through an acute fistula increases, the diameter of only the proximal vein increases, with no change in the antegrade flow in the distal vein [3, 6].
Acquired iliocaval AVF is difficult to treat surgically because of the risk of massive hemorrhage. The morbidity associated with operative repair of AVFs and continuous advances in endovascular techniques and device design have increased the use of endovascular treatment for AVFs. In fact, endovascular therapy has become the treatment of choice for stable patients with suitable anatomy [7]. McCarter et al. first reported the endovascular treatment of an AVF following lumbar disc surgery in 1996 [8]. Many case reports have been published recently, and most authors have reported that endovascular repair should be the first line of treatment of AVF in those patients [9]. A stent graft provided a solution to this difficult iatrogenic injury with low morbidity [10].
We performed endovascular repair using an Endurant stent graft. A stent was deployed without immediate complications, and the AVF was successfully sealed off. Surgical and endovascular repair of a large AVF can lead to dramatic hemodynamic changes. An immediate rise in systemic vascular resistance, decrease in central venous pressure, and decrease in central mixed venous oxygenation can occur. Our patient had an IVC with a 7 cm diameter and a right lower limb DVT. We were concerned about the stent graft patency owing to weak inflow. Therefore, we decided to create a limited inflow fistula between the femoral vein and femoral artery to promote venous patency. We closed it after 3 months. The patient’s symptoms dramatically improved after 6 months.
In conclusion, a 39-year-old patient with high-output heart failure owing to the development of an AVF after iatrogenic lumbar discectomy arterial injury was successfully treated by using an endovascular technique. Six months after the endovascular repair, the patient’s symptoms of heart failure including exertional dyspnea and orthopnea were resolved. Resolution of the dilated heart chambers, a decrease in the diameter of the IVC, and a decrease in pulmonary pressures were also observed.
Conflict of interest statement
None declared.
Funding
There were no funding sources.
Consent
Written informed consent was obtained from the patient for the publication of this case report.
REFERENCES
- angiogram
- orthopnea
- arteriovenous fistula
- jugular venous pressure
- computed tomography
- dyspnea
- leg deep vein thrombosis
- heart failure
- physical examination
- pathologic fistula
- hepatomegaly
- iliac artery
- surgical procedures, operative
- inferior vena cava
- leg
- massive hemorrhage
- exertional dyspnea
- endoluminal grafts
- pitting edema
- lumbar intervertebral disc
- endovascular procedures



