-
PDF
- Split View
-
Views
-
Cite
Cite
Augusto Striano, Francesco Esposito, Francesco Crafa, Leiomyosarcoma of the superior mesenteric artery: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz308, https://doi.org/10.1093/jscr/rjz308
Close - Share Icon Share
Abstract
Arterial leiomyosarcoma (A-LMS) is a very rare tumour and no cases originating from the superior mesenteric artery (SMA) have been described. We present a case of A-LMS originating from distal part of SMA and incorporating superior mesenteric vein (SMV). SMA and SMV were prepared along their course by laparotomy. Prior to resection, the superior mesenteric vessels were clamped, and intra-operative infrared angiography after intravenous injection of indocyanine green was performed. Once confirmed the vitality of the bowel, mass resection including the distal portion of the SMA and SMV was executed. The postoperative course was uneventful. Histology confirmed initial diagnosis. Six months after surgery no recurrence was highlighted. This is the first case of A-LMS originating from SMA, successfully treated without any intestinal resection or vascular reconstruction. The use of near-infrared angiography associated with a preoperative angiographic workup is indispensable for the success of the surgery.
INTRODUCTION
Vascular leiomyosarcoma (V-LMS) is a very rare and aggressive tumour entity that usually arises from medium and large calibre vessels such as inferior vena cava, saphenous vein, femoral and mesenteric vessels [1]. Arterial origin, especially from the abdominal arteries, is unusual [2].
Radical surgical excision is the gold standard treatment and in cases of vascular involvement, a vascular graft is usually useful for restoring the flow [3].
We describe a case of V-LMS of superior mesenteric artery (SMA) (A-LMS) treated with resection of superior mesenteric vessels. In our case, vascular reconstruction was not necessary due to the presence of a good vascularization of the bowel confirmed by intraoperative near-infrared angiography after intravenous indocyanine green administration.
CASE REPORT
This case involved a 63-year-old man who had a history of hypertension, psoriasis and atherosclerosis. He referred the appearance of a light epigastric pain and general discomfort. Laboratory tests were normal. Abdominal ultrasonography was negative as well as the esophagogastroduodenoscopy and colonoscopy. Abdominal computer tomography (CT-scan) with contrast showed a solid mass of about 42 × 31 mm in the mesenteric adipose tissue, incorporating the distal part of the SMA and the superior mesenteric vein (SMV) (Fig. 1). A fluorodeoxyglucose positron imaging tomography/computed tomography (CT) showed an increased uptake (SUV 5.2) at the level of the mesenteric mass.
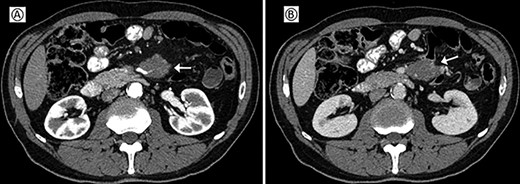
Preoperative CT; (A) arterial phase: the arrow shows the neoplastic mass traversed by the superior mesenteric artery. (B) Venous phase: the arrow shows the neoplastic mass in contact with the superior mesenteric vein.
Surgery was performed through a midline laparotomic approach. The superior mesenteric vessels were isolated throughout their course. Jejunal arteries and veins were prepared and dissected. The mass infiltrated the SMA and the SMV saving the first jejunal vessels, right and middle colic vessels. SMA and SMV were temporarily clamped immediately above the lesion. After intravenous administration of indocyanine green, intraoperative near-infrared angiography (KARL STORZ SE & Co, Germany) showed the good vascularization of the small bowel and the right colon (Fig. 2). An en-bloc resection of the tumour and superior mesenteric vessels incorporated in the lesion was performed without vascular reconstruction, preserving the vessels not affected by the neoplasm (Fig. 3).
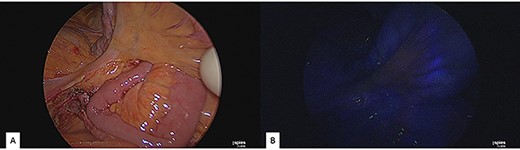
Intraoperative near-infrared angiography and indocyanine green administration; (A) normal light. (B) Application of near-infrared angiography: notice the good vascularization of the small bowel.
![Resection and suture of the superior mesenteric artery and vein; (A) dissection of the superior mesenteric vessels. (B) Superior mesenteric vein sutured distally to the confluence of the ileocolic vein. (C) Superior mesenteric artery sutured distally to the confluence of the ileocolic artery. (D) Superior mesenteric vessels completely sutured. Notice jejunal arteries and veins that have been prepared and dissected. [1] Superior mesenteric artery. [2] Ileocolic artery. [3] Superior mesenteric vein. [4] First jejunal vein. [5] Ileocolic vein. [6] Tumour. [7] Jejunal artery.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2019/11/10.1093_jscr_rjz308/2/m_rjz308f3.jpeg?Expires=1772331645&Signature=eFrXos10pY4wjXCukE~Z6-LOYB7cDG1vK5AG-gDk18rHI21QSVipqdV9zHPKSZkZ~dIIiIpMxptBfpMnDtHCdYLtkKe4UD5Pfxssn6o4BhCvznVtgXssOp3ICSpFD-We-bLT236Dw97eItC3QUsdYuo44asv6gtH8hmwPN7MkwCf5oRecHQN7GXlawf9FoNrHwylbct9alTpKMDxaNW1YsM5v2SlwXq~~HPhd5boQO6DOjtRNg6djN7EJqzIEtxAVR9Rn0HuJbN5yxLNIHg59RdZ6VWpXfrzmqmY3gp67BOt~3fiOOM6Gyxnaq9cT3~KGnsHvihQ-HzmsVG417XV-Q__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Resection and suture of the superior mesenteric artery and vein; (A) dissection of the superior mesenteric vessels. (B) Superior mesenteric vein sutured distally to the confluence of the ileocolic vein. (C) Superior mesenteric artery sutured distally to the confluence of the ileocolic artery. (D) Superior mesenteric vessels completely sutured. Notice jejunal arteries and veins that have been prepared and dissected. [1] Superior mesenteric artery. [2] Ileocolic artery. [3] Superior mesenteric vein. [4] First jejunal vein. [5] Ileocolic vein. [6] Tumour. [7] Jejunal artery.
The postoperative course was uneventful. No bowel suffering or ischemia was highlighted by the abdominal CT-scan on seventh post-operative day (Fig. 4). The patient was discharged on eight post-operative day.
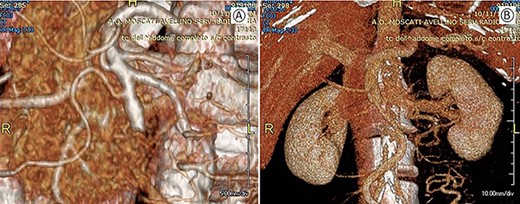
Postoperative CT with 3D vascular reconstruction; (A) arterial phase: superior mesenteric artery with its branches saved. (B) Venous phase: mesenteric-portal axis pervious.
Pathological examination of the surgical specimen confirmed the diagnosis of A-LMS arising from the mesenteric artery also infiltrating the SMV, characterized by foci of coagulative necrosis, immunoreactivity for myogenic markers (smooth muscle actin and desmin, and negativity for S100, C-kit and CD 34), a low number of mitosis (5–10 ×10 HPF) and an high proliferative activity (Ki67) of the tumour cells (30%) (Fig. 5).
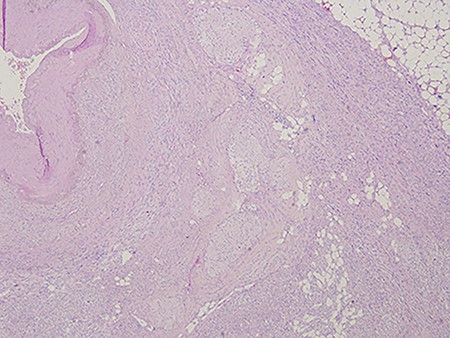
Arterial leiomyosarcoma originating from the superior mesenteric artery; notice the nuclear pleomorphism, mitotic figures and necrotic areas typical of a leiomyosarcoma.
Adjuvant therapy by gemcitabine and docetaxel was performed. A careful radiological follow-up was planned. Three months later, the patient underwent a CT-scan that was negative for local and distant metastases. At the postoperative 6-month follow-up, the patient was symptom-free and no recurrence was detected.
DISCUSSION
We report a case of A-LMS originating from SMA treated with a surgical resection without vascular reconstruction or bowel resection.
V-LMS is an uncommon site of extra-intestinal sarcomas and derives from the smooth muscle cells of the mesenteric vessels [4]. Venous tumours being five times more common than tumours of arterial origin and in the latter cases, it usually affects the peripheral arteries rather than the abdominal ones [5]. Seo HI et al. [2] in a recent review of the literature reported only nine cases of A-LMS originating from intra-abdominal arteries excluding the aorta. Of these, A-LMS was born from the common iliac artery in five cases (55.6%), from the spleno-renal circle in two cases (22.2%), in one case from the right gastroepiploic artery (11.1%) and the same (11.1%) from the inferior mesenteric artery. No case of A-LMS originating from the SMA was reported.
Generally, V-LMS occurs in the middle age and the most frequent symptoms are pain, palpable mass and abdominal distension; occasionally, they can be asymptomatic and can be diagnosed after reaching large dimensions [3, 6]. Angio-CT scan is essential for diagnosis but above all for planning the most appropriate surgical procedure.
The only treatment for this malignancy is an extensive surgical resection, which frequently required a small bowel resection, left or right colectomy or in some cases a multiple organ resection [3,6,7]. A vascular reconstruction with autologous grafts or with prosthesis interposition is sometimes indispensable [3,7].
For the first time, we have applied near-infrared angiography and indocyanine green administration to this type of surgical procedure. This approach avoided a large intestinal resection allowing adequate excision of the neoplastic mass. Near-infrared angiography and indocyanine green are widely used in the assessment of intestinal vascularization, especially in the evaluation of intestinal anastomoses [8], and as demonstrated also in our case, this technique proved to be easy and feasible.
V-LMS usually has a poor prognosis and although there is no definitive evidence on clinical benefits, radiation therapy and adjuvant chemotherapy with various agents are often recommended for local control and in order to reduce the risk of distant metastases [2,3]. Indeed, death is often caused by liver and lungs metastasis [2,9]. In our case, oncologists proposed chemotherapy with gemcitabine and docetaxel; furthermore, a careful clinical and instrumental follow-up was undertaken.
In conclusion, to the best of our knowledge, we are the first to describe a case of A-LMS originating from SMA, successfully treated without any intestinal resection or vascular reconstruction. The use of near-infrared angiography and intravenous indocyanine green administration associated with a scrupulous preoperative vascular radiological workup were indispensable for the ultimate success of the surgery.
Sources of financial support
None.
Conflict of interest statement
None declared.
Availability of data and supporting materials
The authors are responsible of for the accurateness of the presented data and guarantee the full availability of data and materials. Data can be obtained by contacting the corresponding author.
Consent for publication
Written informed consent was obtained by the patient for publication of this article.
Ethical approval and consent to participate
The study was conducted according to the ethical principles of the Institution following the Declaration of Helsinki.



