-
PDF
- Split View
-
Views
-
Cite
Cite
Michelle J Nentwig, Camden M Whitaker, Shang-You Yang, Spinal subdural hygroma as a post-operative complication in revision spine fusion: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz305, https://doi.org/10.1093/jscr/rjz305
Close - Share Icon Share
Abstract
Lumbar spine fusion has become a common and effective procedure in orthopedic practice, and a spinal subdural hygroma development is a rare complication following this procedure. We report here the case of a revision lumbar spine fusion at levels L4-5, L5-S1, where the patient subsequently developed cauda equina syndrome 2 days post-operatively. Magnetic resonance imaging (MRI) showed a subdural, extra-arachnoid fluid collection from T12-L2, cephalad to the site of spine fusion. It appears the first case reported a subdural hygroma developed cephalad to the site of spine fusion. When a patient complains of radicular pain along with urinary retention and neurologic deficits post-lumbar spine surgery, cauda equina syndrome possibly caused by subdural hygroma should be considered. This warrants immediate MRI and emergent reoperation to relieve the pressure on the spinal cord may be necessary.
INTRODUCTION
Lumber spinal surgery for degenerative disorders is a common procedure, with the number of fusions increasing over 70% from 2001 to 2011 [1]. There is a 2–20% incidence of dural tears during lumbar spinal surgery for degenerative conditions [2] . The rate increases when undergoing revision surgery [3]. Subdural hygroma development appears to be a rare occurrence. Only a few case reports of subdural hygroma developed after known durotomy [4 , 5] making this complication uncommon. This case report describes a post-operative complication of cauda equine syndrome with a subdural hygroma that developed cephalad to the site of the spine fusion. To the authors’ knowledge this is the first case reported, whereas previous literature [4] only reporting subdural hygroma at the level of fusion.
CASE PRESENTATION
A 34-year-old male who was admitted for revision L5-S1 and primary L4-L5 decompression and posterolateral instrumented fusion of L4-S1. Eight months prior he had undergone a left sided laminectomy and discectomy of L5-S1 for disk herniation. A few months after his initial fusion procedure, the patient reported falling down a flight of stairs and developed worsening lower extremity pain and radicular symptom. Preoperative imaging 3 months prior to his revision showed recurrent disk herniation at L5-S1 as well as new herniation at L4-L5 (Fig. 1). The procedure went without complication, with no note of durotomy, and the fascia was closed using a bidirectional barbed suture.
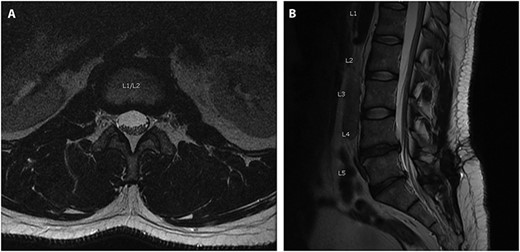
Axial (A) and Sagittal (B) T2 MRI imaging obtained preoperatively when presented for back pain, 8-months after a previous L5-S1 laminectomy/diseconomy. Images here show no evidence of pre-operative subdural fluid collection.
On post-operative day 2, the patient began having urinary retention, bilateral leg pain and numbness in the left L5 distribution. Magnetic resonance imaging (MRI) showed a T12-L2 subdural fluid collection measuring ~8 mm in depth and exerting a mass effect on the distal spinal cord and cauda equina (Fig. 2). The patient was urgently taken back to the operating room for L1-L2 decompressive laminectomy. The thecal sac was under considerable tension and when an incision was made through the dura, the cerebrospinal fluid (CSF) appeared to be under pressure. The epidural space was inspected and no hematoma was noted. A lumbar drain was left in the subdural space. The drain was kept in place for 3 days. The patient progressed well with his strength and sensation, except for some residual numbness in the left toes. The patient was discharged home.
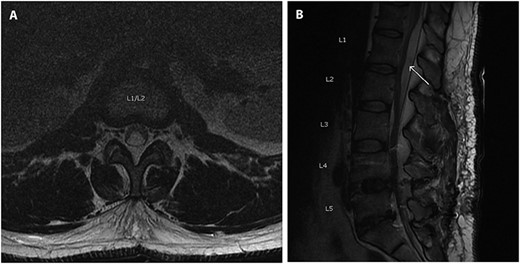
Axial (A) and sagittal (B) T2 MRI scan obtained post-operatively showing a subdural hygroma (arrow), cephalad to the site of fusion, which caused symptoms of cauda equina syndrome.
DISCUSSION
Although relatively rare, an incidental durotomy can happen during spinal procedures such as lumber spine fusion [2, 6]. A subdural hygroma is a collection of CSF that develops between the dura and the arachnoid layers. Although subdural hygromas are common after traumatic brain injuries, they are rare occurrences during spinal and brain surgeries [7]. Baker et al. [8] examined a large number of cases and summarized some risk factors for unintended subdural tear in spinal procedures including age, comorbidities such as diabetes, surgical invasiveness and revision procedures. In most cases, durotomies are identified during the surgery and repaired. There is still a rare incidence of CSF leak after spine surgery [9]. In this reported case, there was no note of durotomy during the revised spine fusion procedure. The preoperative MRI image ruled out the possibility of a pre-existing traumatic arachnoid cyst prior to surgery. The most commonly listed complications of subdural tears, with primary closure or missed dural tears include headache, nausea/vomiting, pseudomeningocele and myelocutaneous fistulas [10]. Two cases of subdural hygroma were reported causing cauda equina syndrome after lumbar surgery in 2012 [4]. In both cases, the patients underwent revision lumbar decompression and inadvertently sustained damage to the dura but no CSF leaks were noticed and in one of the cases the dura was repaired. They proposed that a disruption of the arachnoid layer causes a one-way valve that allows the CSF to enter the subdural space. In another case, a patient who had a repair of Chiari malformation with pinhole disruption of the arachnoid and subsequently developed cauda equina syndrome and was found to have a subdural, extra-arachnoid, CSF fluid collection at L2-L5 [5].
Of note, none of the case reports discussed the technique used to close the fascia in the initial surgery. In this reported case, a running bidirectional barbed suture was used to close the fascia. Although barbed suture is common practice in many specialties like plastic surgery, urology and obstetrics, there is little research on the safety and effectiveness in spine surgery. Some of the benefits for using barbed suture include cost/time saving [11] and the ability to get a tight fascial closure, an important component of preventing complications when durotomy can occur, given the fact that this case had higher risk as a revision procedure. However, our postulation is that over tightening of the barbed suture may have prevented a CSF leak at the surgical site but causing the CSF to migrate proximally in the subdural space.
The presentation of cauda equina symptoms typically includes patient’s complaints of lower back and leg pain followed by symptoms of urinary retention [12]. It is imperative that MRI imaging be obtained for diagnosis. Of the four case reports, including ours, each was treated with immediate surgical intervention. Two of the three were treated with decompression and no mention of drain placement. In the case reported by Singleton et al. [4] a lumbar drain was placed in the subdural space. In our case, the patient underwent immediate surgical exploration with the placement of a subdural lumbar drain. As with our case, each of these patients had complete resolution of their symptoms.
CONCLUSIONS
Although rare in occurrence when a patient presents with radicular pain, urinary retention and neurologic deficits the surgeon should be alerted to cauda equina syndrome possibly caused by subdural hygroma. This warrants immediate MRI imaging. While there are no guidelines for the preferred methods of treatment, emergent reoperation to relieve the pressure on the spinal cord is necessary.
CONSENT
The patient has given verbal consent to report his case without release of protective personal information. The institutional human investigation review board exempts single case report. All authors declare that they have no competing interests.



