-
PDF
- Split View
-
Views
-
Cite
Cite
John Alfred Carr, Acute fulminant necrotizing mesenteric lymphadenitis causing bowel ischemia, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz304, https://doi.org/10.1093/jscr/rjz304
Close - Share Icon Share
Abstract
This case report documents the medical progression of a 56-year-old man who presented with a small bowel obstruction and was found to have acute fulminant necrotizing mesenteric lymphadenitis causing small intestinal ischemia. A large portion of the proximal jejunal mesentery was necrotic with vascular thrombosis leading to small bowel ischemia and obstruction. He was successfully managed surgically and survived. The evaluation and possible aetiologies are discussed.
INTRODUCTION
Mesenteric lymphadenitis commonly occurs in children and is an inflammatory and self-limited disease, which usually resolves within 4 weeks [1]. Although rare in adults, infectious lymphadenitis can progress to complete necrosis of the mesenteric lymph nodes if the infection is due to tuberculosis, Yersinia or salmonella infection [2]. This case report documents the medical progression of a 56-year-old man who presented with an acute small bowel obstruction and was found to have acute fulminant necrotizing mesenteric lymphadenitis causing small intestinal ischemia. The findings and management are discussed.
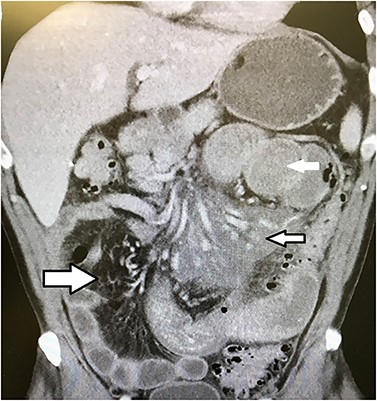
CT scan of the abdomen showing dilated proximal small bowel (solid white arrow), inflammatory changes in the proximal small bowel mesentery around the superior mesenteric artery (small black and white arrow) and normal distal mesenteric fat (large black and white arrow).
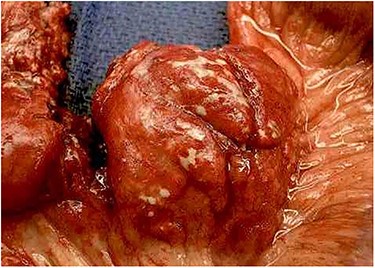
A large necrotic mesenteric lymph node with a ruptured capsule showing purulent drainage.
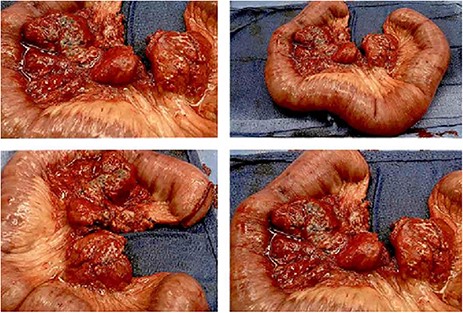
The entire excised specimen showing all of the enlarged necrotic lymph nodes and ischemic bowel.
CASE REPORT
A 56-year-old man presented to the emergency department with 5 days of abdominal pain, diaphoresis, nausea and vomiting. He had been unable to tolerate any food for the previous 48 hours. He was otherwise healthy and took no medications. He had no history of prior surgery.
On physical examination, he was mildly tachycardic, diaphoretic, normotensive and had a mildly distended abdomen with diffuse tenderness without peritoneal signs. Laboratory results showed a mild leukocytosis with a white blood cell count of 14 K and hypochloraemia, hyponatraemia and hypokalaemia. After intravenous fluid resuscitation, computed tomography of the abdomen showed very dilated proximal small bowel and stomach with extensive inflammatory changes and fat stranding throughout the proximal mesentery (Fig. 1). The distal and colonic mesentery appeared normal.
He was admitted to the hospital for electrolyte replacement, and a nasogastric tube was placed to decompress the bowel. The following day his electrolytes had normalized, but his WBC had elevated to 16 K, and he developed peritonitis.
Emergent laparotomy was performed. He was found to have multiple enlarged necrotic mesenteric lymph nodes with purulent material draining from the capsule of the nodes (Fig. 2). Several large areas of the proximal mesenteric fat were necrotic with vascular occlusion and thrombosis, which was causing ischemia of the proximal jejunum. The proximal jejunum was very dusky and dilated, while the distal small bowel and colon was normal. The duodenum was spared. The necrotic fat and lymph nodes extended down to and around the superior mesenteric artery, where multiple side branches off the artery showed no blood flow by Doppler examination. The ischemic small bowel was excised along with its mesentery down to the superior mesenteric artery, to include the excision of the necrotic lymph nodes (Fig. 3). The bowel was left in discontinuity, and the patient was taken to the intensive care unit with a temporary abdominal closure. He was taken back to the operating theatre the next day for a second look, and the remaining small bowel was found to be viable and healthy. A duodenal to distal jejunal anastomosis was performed and the abdomen was closed.
The patient made a rapid recovery and was discharged on hospital day six. The pathology report documented multiple enlarged and necrotic lymph nodes with necrotic mesenteric fat and vascular occlusion, as well as ischemic changes to the intestine. No malignancy was identified. The lymph nodes did not show non-caseating granuloma formation or other granulomas within the nodes. All blood cultures and the operative cultures of the purulent lymph nodes failed to show any bacterial or viral growth. The cultures were also negative for the tuberculosis and fungi. Since the necrotizing process appeared to be non-infectious, an extensive autoimmune work-up was later performed, which was only weakly positive for rheumatoid factor. Double-stranded DNA antibodies, anti-nuclear antibodies, anti-phospholipid antibodies and sedimentation rates were normal. Rheumatology consultation did not result in any additional treatment. The patient was seen back in the office for 6-month and 1-year follow-ups and was back to work and had no recurrence and no additional problems.
DISCUSSION
With the exclusion of tuberculous mesenteric lymphadenitis, other causes of necrotizing mesenteric lymphadenitis leading to abdominal complications in the adult are very rare, with only three cases reported in the literature [3–5]. The necrotizing process in these cases was due to systemic lupus erythematosus in one, Still’s disease in one, and unknown in the other. Unlike these patients, the patient described in this case report had a negative autoimmune work-up and did not have any rash, arthritis or symptoms of an autoimmune disorder either before or after his hospitalization. Although autoimmune disease was suspected, it could not be proven; other than the weakly positive rheumatoid factor, which the rheumatology consultant did not think was relative.
Another sterile necrotizing lymphatic disease that often affects the cervical lymph nodes is Kikuchi–Fujimoto disease (KFD). This disease is often mistaken for cervical tuberculous adenitis. Although almost exclusively occurring in the neck region of children, three cases of KFD have been reported in the mesenteric lymph nodes of adults [6–8]. Two were diagnosed during surgery for presumed appendicitis, and one by biopsy. KFD has a classic histiocytic necrotizing inflammatory process within the lymph nodes, which can be confirmed by immunohistochemistry [8]. But none of those patients had disease so extensive as to cause mesenteric ischemia, and the patient in this report did not have immunohistochemistry consistent with KFD. The exact aetiology of what led to the necrotizing mesenteric lymphadenitis in this patient remains a mystery.
ACKNOWLEDGEMENTS
The author does not have any conflict of interests and did not receive any financial support for this work.
CONFLICT OF INTEREST STATEMENT
None declared.



