-
PDF
- Split View
-
Views
-
Cite
Cite
Jing Wang, Matthew Ng, Kunal Kochar, Large presacral abscess in a patient with Crohn’s disease, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz297, https://doi.org/10.1093/jscr/rjz297
Close - Share Icon Share
Abstract
A presacral abscess with sacral osteomyelitis and gluteal abscesses is a very rare complication of Crohn’s disease and is often clinically unsuspected or overlooked. We report a case of a 58-year-old male who presented for right hip pain after a fall. An abdominal and pelvic CT scan showed an atypical presacral abscess with a fistulizing tract extending through the sciatic notch and lateral to the gluteus medius and minimus muscles forming an intramuscular abscess. The endoscopic transanal approach was used to drain the presacral abscess. This method of drainage was successful and the patient had a favorable prognosis.
INTRODUCTION
A presacral abscess is a rare complication of Crohn’s disease, and it can fistulize to form abscesses in nearby organs. About 10–30% of patients with Crohn’s disease will develop an abdominal or pelvic abscess spontaneously over their lifetime, but usually as a post-operative complication [1], and only a small percentage of these are presacral in origin. Possible drainage methods cited in the literature for pelvic abscesses include CT- or ultrasound-guided transgluteal, transperineal, percutaneous, transvaginal, transpedicular and paracoccygeal-infragluteal approaches. The case here explores this unique presentation of a presacral abscess due to a low posterior rectal perforation secondary to active Crohn’s disease and its management.
CASE REPORT
A 58-year-old male with a history of Crohn’s disease, irritable bowel syndrome and Clostridium difficile presented after falling on ice and developing right hip pain with localized right thigh swelling. X-rays of his chest, femur, hip and knee were all unremarkable.
CT abdomen and pelvis showed a rectal perforation with perirectal pelvic inflammatory soft tissue/phlegmon containing air-fluid level that infiltrated into the presacral space extending up through the sciatic notch into the right gluteus medius and minimus muscle (Figs 1 and 2). Chronic inflammatory changes of the transverse colon and left colon were also present. The patient was taken to the operating room (OR) for examination under anesthesia. A flexible sigmoidoscopy was passed up into the distal descending colon, which showed discontinuous areas of ulcerated mucosa with cobble-stoning notable for active Crohn’s disease and a diffuse pseudomembrane reminiscent of C. difficile colitis (the negative C. difficle assay). A rectal perforation was noted just above the dentate line. The incision was enlarged and the presacral space was entered with a flexible sigmoidoscope. There was extensive necrosis of the presacral tissue with copious amounts of purulent fluid. The abscess was evacuated, and all loculated fluid collections were drained. The cavity was then irrigated via the sigmoidoscope. Once satisfactory drainage was achieved, a Malecot catheter was then inserted through the rectal perforation into the presacral space. A laparoscopic diverting loop ileostomy was then created to allow for healing.
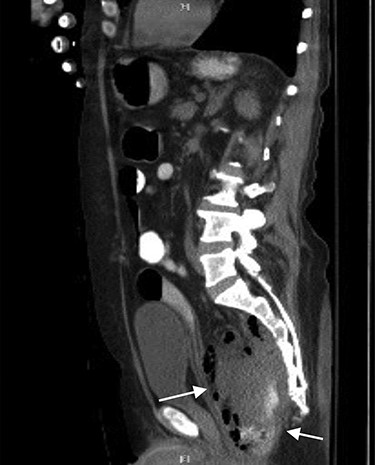
CT sagittal view showing contrast (white) entering the lumen of presacral abscess and rectus abdominis muscle pushed anteriorly.

CT axial view showing tract from presacral space through the sciatic notch to thigh muscles.
Marked improvement was seen on CT post-operative day 5 (Fig. 3). MRI of the pelvis showed marrow edema in the sacrum and coccyx, which was consistent with osteomyelitis and complex fluid collections of the right pelvis and right upper thigh, which was likely tracking from the presacral process. A CT guided drain placement was done for the right thigh abscess. Repeat MRI on day 14 showed resolution of the pelvic abscess, sacral osteomyelitis and myositis of the left gluteal and iliacus muscles. The patient was taken back to the OR to remove the rectal drain and replace it with a transperineal drain. This was carried out to allow the rectal perforation to heal and to provide continued drainage given the persistent myositis and osteomyelitis. The patient was started on steroids for his Crohn’s disease with plans to switch to biologic therapy. The transperineal drain was removed on post-operative day 25, and he was discharged home on biologic therapy with tapering of his steroid regimen.
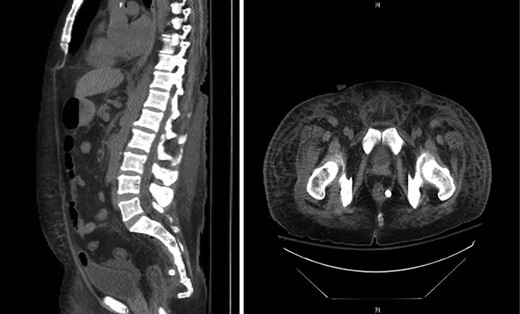
Computed tomography (sagittal and axial views) showing post-operative resolution of the presacral abscess (post-operative day 5).

Flexible sigmoidoscopy demonstrating granulation tissue at the posterior aspect of the distal rectum.

External view at post-operative day 65 demonstrating a right lateral subcutaneous fistula-in-ano with a seton in place. At the posterior midline, is granulation tissue from prior transperineal drain placement.
After 8 weeks, the patient was taken for repeat examination under anesthesia and flexible sigmoidoscopy. There was a significant improvement in the severity of his Crohn’s colitis. The rectal perforation had closed (Fig. 4) and the transperineal wound had completely healed. Once the Crohn’s disease is adequately controlled with medical therapy, the ileostomy will be addressed (Fig 5).
DISCUSSION
Pelvic abscesses develop in patients with Crohn’s disease due to the transmural inflammation causing a contained perforation leading to abscess formation [1]. Presacral abscesses as a complication of Crohn’s disease is extremely rare. Furthermore, sacral osteomyelitis as a complication of this abscess is also exceedingly rare and possibly due to a direct extension of the fistula into bone or erosion into the bone of a contiguous deep abscess [2]. Usually pelvic abscesses and osteomyelitis occur in patients with long-standing fistulizing entero-colic Crohn’s disease averaging 4 years of disease history [3,4]. The presacral space can be one of the more difficult locations to drain and the percutaneous anterior abdominal approach has been most commonly used; however, that approach carries dangers of vascular or neural damage [1]. Other methods include ultrasound and CT-guided transgluteal, transvaginal and precoccygeal drainage. [5,6].
A similar drainage approach was detailed in a case report on a 37-year-old with sepsis presenting with a post-operative pelvic abscess following a Hartmann procedure for perforated rectal cancer. Percutaneous drainage was unsuccessful, so a transrectal endoscopic drainage was accomplished, which allowed visualization of the local cavity, drainage and saline irrigation [6]. Similarly, in our case report, the fistula tract opening was visualized in the anal canal on flexible sigmoidoscopy, so the scope was advanced into this opening, purulent material was drained and the presacral space was visualized to place the Malecot catheter. We believe this is an appropriate minimally invasive method of initial drainage of presacral abscess. Once the abscess resolves, the rectal drain should be removed to allow for healing of the rectal perforation, as the Crohn’s colitis improves on medical management. These patients will also require a proximal diversion of the fecal stream to achieve healing.
To the best of our knowledge, our report is the first description of a direct endoscopic transanal drainage for a presacral abscess in a patient with active Crohn’s disease. Our results show that this method is safe and an effective alternative to other drainage approaches. It is crucial for physicians to keep in mind atypical presentations of complications of Crohn’s disease and to pick an abscess drainage technique that has ease of access and causes the least damage to surrounding anatomic structures.
CONSENT FOR PUBLICATION
The patient consented for publication of this case report and any accompanying images.
ACKNOWLEDGMENTS
We would like to thank our family and friends for their continued support.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was received for this article.



