-
PDF
- Split View
-
Views
-
Cite
Cite
Rupesh Kumar, Javid Raja, Sanjib Rawat, Ayush Srivastava, Shyam Kumar Singh Thingnam, Chronic constrictive pericarditis complicated with huge right atrial thrombus in a child with abdominal tuberculosis: a rare life-threatening condition, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz295, https://doi.org/10.1093/jscr/rjz295
Close - Share Icon Share
Abstract
Chronic constrictive pericarditis (CCP) is the most common pericardial pathology. CCP complicating with intracardiac thrombus is a rare entity, the detection of thrombus preoperatively is life-saving in avoiding the risk of pulmonary thromboembolism during anterior pericardiectomy. Transesophageal echocardiography has been shown to have better sensitivity in detecting atrial thrombus than transthoracic echocardiography. Surgical removal of right atrial thrombus under cardiopulmonary bypass should be considered.
INTRODUCTION
Chronic constrictive pericarditis (CCP) is a common pericardial pathology. Its association with intracardiac thrombus is uncommon. Intracardiac thrombus may embolize to great vessels leading to life-threatening events. It can easily be diagnosed by transesophageal echocardiography, which will guide us whether opening of cardiac chamber is needed and hence the need of cardiopulmonary bypass. Multiple comorbidities such as tuberculosis, poor growth and cardiac cachexia complicate the clinical outcome associated with CCP and hence necessitate more vigilant work-up and intervention planning for better outcome. Most of the surgeries for CCP are conducted nowadays without the aid of cardiopulmonary bypass, whereas those complicated by intracardiac thrombus necessitate the use of cardiopulmonary bypass, and such provision of CPB (cardiopulmonary bypass) should be available in centers performing surgery for this clinical condition. The initiation of CPB is challenging in these cases due to adhered and thickened pericardium over the heart.
CASE REPORT
A 7-year-old male child got admitted to pediatric emergency ward with symptoms of breathlessness since 3 days. He was emaciated, febrile, pale, engorged neck veins, ascites with tensed abdomen without any pedal edema. Chest auscultation revealed diminished breath sounds on left side of the chest with muffled heart sounds. He was on drugs for abdominal tuberculosis for the last 2 months. A chest X-ray revealed left-sided pleural effusion, few calcific nodules on left hilar region with calcific heart borders. Ascitic fluid tap was done and around 2 l of amber colored fluid was drained out. The sample had raised adenosine deaminase level without any mycobacterium on routine examination of the centrifuged sample of the fluid. An urgent transthoracic echocardiography (TTE) was done, which revealed thickened pericardium, paradoxical movement of interatrial septum and hepatic flow reversal of blood during cardiac cycle suggesting constrictive pericarditis. Contrast-enhanced computer tomography (CECT) of thorax revealed thickened calcified pericardium with left-sided pleural effusion. The child was planned for anterior pericardiotomy next morning following routine work-up. Preoperative transesophageal echocardiography (TEE) on operation table showed an echogenic mass in right atrium, suggesting huge thrombus that was not detected on echocardiogram as well as on CECT. Hence, a plan to consider anterior pericardiectomy with the aid of cardiopulmonary bypass was made to remove thrombus from the right atrium. The anterior pericardium was very thick, whitish and glistening, suggesting a long-standing pathology (Fig. 1). Anterior pericardiectomy extending from just below the course of innominate vein till its joining the diaphragm and bilaterally limited till the phrenic nerves was performed. The operation was uneventful with satisfactory postoperative outcome and smooth recovery. He is on follow-up for the last 2 years without any symptoms of breathlessness or ascites.
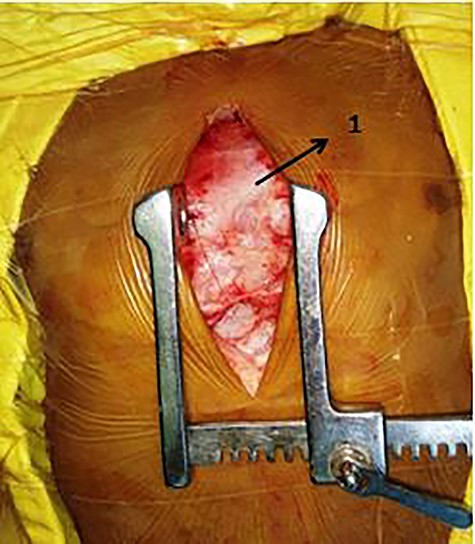
Intraoperative picture of thickened pericardium (1—thick, whitish and glistening anterior pericardium).
DISCUSSION
CCP is the most common pericardial pathology in developing countries, the most common causative factors being tuberculosis [1]. CCP complicating with intracardiac thrombus is rare, the detection of thrombus preoperatively is life-saving in avoiding the risk of pulmonary thromboembolism during anterior pericardiectomy [2]. Right atrial thrombus is uncommon and usually found in patients with right-sided cardiac abnormalities or foreign bodies [3,4]. The association of atrial thrombus with CCP was first reported in 1987 [3].
Two main causes of intracardiac thrombi include blood stasis and endocardial injury of the heart. In constrictive pericarditis, impairment of ventricular filling during diastole causes intracardiac stasis of blood, which is considerably worsened by the presence of atrial fibrillation, in turn causing thrombus formation [4]. In addition, myocardial involvement in association with pericarditis leads to an endocardial inflammatory process, thereby facilitating thrombosis [4].
Right atrial thrombi detected by echocardiography are of two types. Type 1 thrombus is with long, thin and extremely mobile thrombi and is associated with early mortality in 42% patients. Type II thrombus is an immobile, nonspecific clot and is associated with early mortality in only 4% patients [5]. TEE has been shown to have better sensitivity in detecting atrial thrombus than TTE [6]. Computer tomography and magnetic resonance imaging can demonstrate generalized pericardial thickening and pericardial calcifications as well as the morphology of the thrombus when present [7].
Treatment of right atrial thrombus depends upon the etiology and morphology of the thrombus. Thrombolysis is an option for type 1 thrombus [8]. Giant atrial thrombi are not amenable to thrombolysis, which might lead to fatal complications [9]. Hence, the decision for thrombolysis or surgical removal is taken on an individual basis depending on the morphology of the thrombus and clinical condition of the patient [10].
Right atrial thrombus might be associated with constrictive pericarditis more commonly than previously recognized. The clinical features can be masked by those of cardiac constriction; however, the presence of thrombus within the right atrium has important clinical and therapeutic implications. Surgical removal of right atrial thrombus should be considered because of the associated morbidity and mortality.
Conflict of Interest
None declared.
Funding
No source needed for this study.
References
- pericardial sac
- cardiopulmonary bypass
- transesophageal echocardiography
- atrial thrombus
- intracardiac thrombosis
- child
- pericardiectomy
- tuberculosis
- abdomen
- pathology
- thrombus
- echocardiography, transthoracic
- thromboembolism, pulmonary
- chronic constrictive pericarditis
- right atrial thrombus
- excision
- clear cell papulosis



