-
PDF
- Split View
-
Views
-
Cite
Cite
Lei Ying, Jeong-Moh John Yahng, The rare case of De Garengeot hernia: femoral hernia containing perforated appendicitis, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz287, https://doi.org/10.1093/jscr/rjz287
Close - Share Icon Share
Abstract
Femoral hernias account for ~4% of all groin hernias but are much more common in females, especially those over the age of 70. Risk of incarceration is overall low but can include structures such as bowel, omentum, bladder, ovary and very rarely, the appendix. The subset of femoral hernias containing the vermiform appendix is known as de Garengeot hernias. We describe a rare case of an 87-year-old female patient who presented with an incarcerated right femoral hernia confirmed on contrast-enhanced computed tomography scan of the abdomen and pelvis, with subsequent open hernia reduction revealing a perforated necrotic appendix with pus contained in the hernia sac. Histopathology revealed acute appendicitis with increased stromal fibrosis suggestive of a chronic process. Pre-operative diagnosis of de Garengeot hernias remains challenging due to their non-specific presentation and attenuated clinical symptoms, and most diagnoses are made intraoperatively.
INTRODUCTION
Femoral hernias represent ~3–4% of all groin hernias with a female preponderance, of which ~0.5–5% involves the migration of the appendix through the femoral canal and is termed de Garengeot hernia, named after Rene Jacques Croissant de Garengeot (1688–1759), a Parisian surgeon who first described the rare phenomenon [1]. Since then, <100 cases have been reported in the literature [2]. The presence of acute appendicitis within a femoral hernia is even rarer still, with an incidence of 0.08–0.13% described in the literature [3]. We present a rare case of an 87-year-old lady who presented with an incarcerated right femoral hernia containing a perforated necrotic appendix and our surgical management.
CASE REPORT
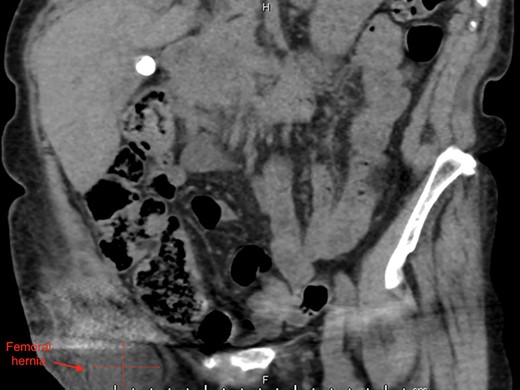
An 87-year-old Caucasian female presented to the emergency department with a 5-day history of worsening right groin pain, with an associated 2-day history of generalized malaise and fatigue. She denied fever, nausea and vomiting or signs of bowel obstruction. Her past medical history included previous right total hip replacement, type 2 diabetes mellitus and chronic renal impairment. Her vitals were normal, and examination revealed a tender right groin lump below the level of the pubic tubercle approximately 4 × 4 cm in size, with overlying erythematous skin changes. Biochemical investigation revealed a normal white cell count of 10.0 × 109/L and neutrophil profile of 7.8 × 109/L but an elevated C-reactive protein (CRP) of 190 mg/L. Contrast-enhanced computed tomography (CT) scan revealed a hypodense rounded lesion measuring 3.8 × 4.3 × 3.1 cm, medial to the right femoral vessels and extending lateral to and below the level of the pubic tubercle in the proximal anterior thigh, most consistent with a incarcerated femoral hernia (Figs. 1–3). The presence of right total hip replacement artifacts precluded accurate assessment for communication of the lesion with the peritoneal cavity.
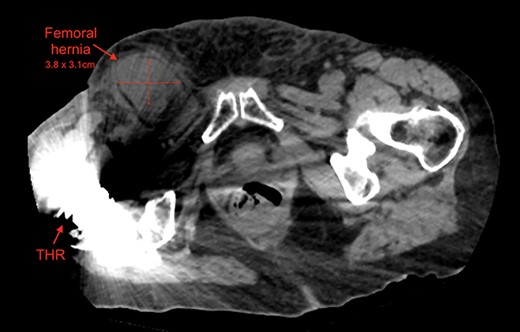
Axial view of right femoral hernia, note the significant image distortion from the right total hip replacement beam artifacts.

The patient was urgently taken to the operating theater for surgery under general anesthesia. An open oblique incision was made over the right groin lump via Lockwood low approach. Dissection in layers revealed a large hernia sac inferior to the inguinal ligament resembling a femoral hernia which was unable to be reduced from below. A second more horizontal skin incision was made superiorly above the level of the inguinal ligament via McEvedy high approach. The hernial sac was then excised to reveal an abundance of pus and necrotic tissue forming the perforated tip of an inflamed and dilated appendix (Fig. 4). An open appendicectomy was performed, the right femoral hernia sac was resected and the femoral defect was closed inferiorly, with the repair allowing passage of a fingertip space. Postoperatively, the patient received 48 hours of intravenous antibiotics. She recovered uneventfully and was discharged on post-operative Day 5. Histopathological examination revealed acute appendicitis with a swollen vermiform appendix measuring 42 × 15 × 19 mm with purulent exudate and haemorrhagic serosal surface with increased fibrosis consistent an inflammatory process of some weeks in duration.
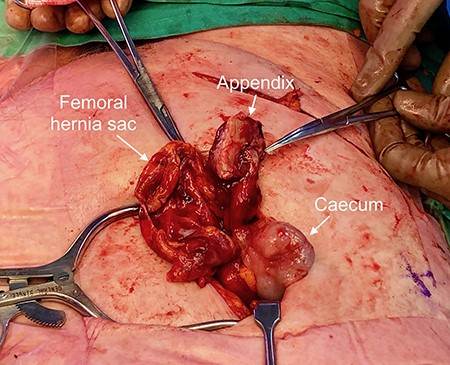
Macroscopic view of the open surgical field pointing toward patient feet. The McEvedy high incisional wound containing contents: right femoral hernia sac, perforated inflamed appendix and part of the caecum.
DISCUSSION
The major risk factors for developing de Garengeot hernias included being older age, female gender (3:1 ratio) including post-menopausal status and pregnancy-related changes, smoking, constipation and chronic cough [4]. Proposed theories for how de Garengeot hernias develop include the mass effect from an anatomically large caecum pushing the appendix into the femoral canal [5] to abnormal rotation of the mid and hindgut during embryological development increasing the propensity of the appendix to herniate through the femoral canal [6].
The mechanism for which appendicitis develops inside the femoral canal is also contentious, whether the appendix migrates into the narrow, rigid femoral ring where it then becomes incarcerated and strangulated or appendicitis occurs first followed by its migration into the femoral canal [7]. We contend the former to be more plausible, as the femoral hernia sac confers a relatively contained anatomy where the appendix may gradually incarcerate and develop chronic inflammation without irritation to the bowel and other surrounding structures. In our histological specimen, there was an absence of faecalith, but evidence of haemorrhagic serosal surface with increased fibrosis indicating a more chronic inflammatory process suggesting the appendix may have resided in the femoral canal for some time before developing infection.
The pre-operative diagnosis of de Garengeot hernias is made difficult by its non-specific clinical presentation and attenuated symptoms. Patients usually present with a painful right-sided groin lump without the systemic symptoms of fever, tachycardia, nausea, vomiting associated with intraperitoneal pathology as the nature of the femoral canal tends to limit the spread of sepsis into the peritoneal cavity [8]. Thus, even perforated appendicitis tends to manifest as localized tenderness rather than generalized peritonitis, delaying the patient’s presentation.
Imaging modalities also vary in their ability to detect de Garengeot hernias, with MRI being the most sensitive but usually reserved for young pregnant women [9]. Ultrasonography is useful in non-obese patients but is operator-dependent. Hence, CT scan remains the modality of choice as it can at the very least detect a herniating mass projecting below the caecum into the femoral canal with fat stranding [10]. In our case, we relied on CT evidence of possible incarcerated femoral hernia along with a raised CRP of 190 mg/L to influence our decision for surgical intervention.
We attempted the femoral hernia reduction using the Lockwood low approach initially, without confirmation of the presence of the appendix within the femoral sac. When the hernia sac was irreducible, a second incision higher up using the McEvedy high approach was able to reduce the hernia after division of the lacunar ligament. Confirmation of the diagnosis of de Grengeot hernia was made after excision of the hernia sac revealed the contents of pus and necrotic tissue forming the perforated tip of an inflamed dilated appendix. Although the infra-inguinal low approach was the preferred method in elective hernia repair, it has the disadvantage of limited access if the viscera is compromised and offers little scope for resecting any compromised bowel. The McEvedy high approach was the preferred method in the emergency setting when strangulation is suspected allowing better access to and visualization of bowel for possible resection [4].
ACKNOWLEDGEMENTS
Not applicable.
FUNDING
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
CONSENT FOR PUBLICATION
Written formal consent was obtained from the patient for publication of this case report and accompanying images.
COMPETING INTERESTS
The authors declare that they have no competing interests.



