-
PDF
- Split View
-
Views
-
Cite
Cite
Chiapo Lesetedi, Mpapho Joseph Motsumi, Forgotten metal stent (3 years) presenting with a high burden of intra- and extra-hepatic ducts stones and cholangitis, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz294, https://doi.org/10.1093/jscr/rjz294
Close - Share Icon Share
Abstract
Forgotten stents may lead to serious complications. We present a case report of a forgotten common bile duct (CBD) fully covered metal stent presenting with recurrent cholangitis. A 79-years-old female patient presented with a history of recurrent cholangitis. Past surgical history was notable for open cholecystectomy for symptomatic cholelithiasis in 2016. Subsequently, she was found to have retained CBD stones in the same year. She had endoscopic retrograde cholangiopancreatography (ERCP), during which a complete clearance of the stone was not achieved and she was stented with a completely covered metal stent. She was lost to follow-up until 2019. A differential diagnosis of cholangitis secondary to a blocked stent was made. At ERCP, she had intra- and extra-hepatic stones, which could not be removed. A plastic stent was deployed. She later had an open bile duct exploration with Roux-en-Y hepaticojejunostomy. Forgotten stents can lead to serious complications. An electronic stent follow-up registry is recommended.
INTRODUCTION
The patients’ adherence to stent follow-up schedule is critical. Forgotten or stents retained in the biliary ducts for a prolonged period without follow-up can lead to serious complications.
CASE REPORT
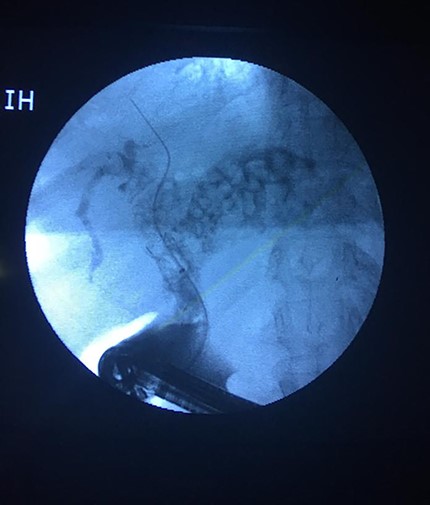
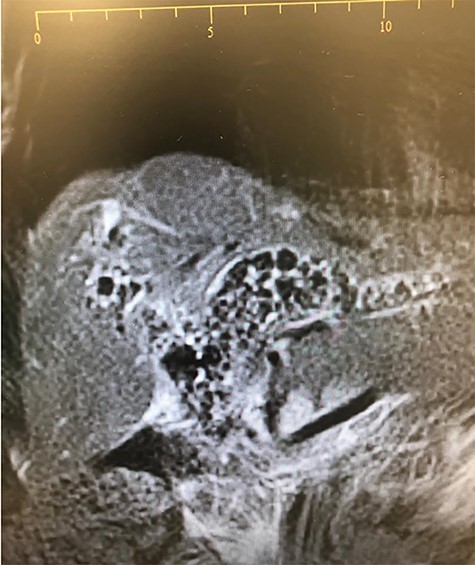
We present a 79-years-old female patient who presented on the 31 January 2019 with worsening recurrent right upper quadrant pain, dark urine, chills and tiredness for 12 months. She was a known diabetic and hypertensive controlled on medications. Her past surgical history was notable for having had an open cholecystectomy for symptomatic cholelithiasis in 2016. The same year post cholecystectomy, she was found to have retained common bile duct (CBD) stones. She had endoscopic retrograde cholangiopancreatography (ERCP), during which a complete clearance of the stone was not achieved and she was stented with a completely covered metal stent. There was no follow-up until she got symptomatic in 2019 and she presented with cholangitis. Her blood workup showed an obstructive picture. The abdominal ultrasound was not diagnostic. She was started on analgesia and antibiotics. A differential diagnosis of a blocked stent was made. She had an ERCP on the 04 February 2019. An old stent was found, which could not come out. An extraction balloon was used to clean the old stent of debris and small stones and a 10 Fr × 9 cm plastic stent was deployed. On table, cholangiogram showed dilated ducts with multiple stones in the CBD extending into the left and right hepatic ducts and the first order ducts bilaterally (Fig. 1). MRCP confirmed the cholangiogram findings (Fig. 2). On 18 February 2019, she had open bile duct exploration and Roux-en-Y hepaticojejunostomy reconstruction (wide anastomosis). The stents and multiple stones were removed (Fig. 3). She had an uneventful post-operative course. At her first follow-up, 6 weeks later, she had normal liver function tests and felt much better.

DISCUSSION
In patients with gallbladder stones, 10–15% of them will have concomitant CBD stones [1]. Rarely bile duct stones may form primarily as intrahepatic or extrahepatic stones without originating from the gallbladder. CBD stones originating from the gallbladder are called secondary bile duct stones and those that formed primarily in the biliary ducts are called primary bile duct stones [1–3]. Risk factors for gallstone formation are nutrition, obesity, weight loss, female sex, race and serum lipid levels. Primary intrahepatic stones are common in Asia and studies suggest that parasitic infestation may play a role [1, 2]. A combination of bile infection, dietary factors, biliary stasis, and possibly parasitic infestation are implicated in the formation of intrahepatic biliary stones [2].
Patient with forgotten stents commonly present with abdominal pains, obstructive jaundice and cholangitis. They usually have deranged liver function tests and dilated biliary tracts on abdominal ultrasound [1, 4, 5]. Biliary stents are foreign bodies and, therefore, form a nidus of infection particularly if not removed within 4–6 weeks from insertion [3, 4]. The de novo formation of biliary stones around the stent was reported in a few case reports [1, 4]. These may lead to a stone-stent complex assuming a lollipop, dumb-bell, or the stent shape [1, 4]. Bansal and his colleagues were the first to term this complex ‘stentolith’ in 2009 [4].
Our case had a rather rare finding with stones extending from the CBD, into the right and left hepatic bile duct and the first-order intrahepatic biliary ducts on both sides. Most of the reported cases had only CBD stones [1, 4, 5]. This was the first case with such an extensive biliary tree involvement with stones. The real cause of the burden of stones in the biliary tract is unknown. It is noted, however, that our case was the only one reported with a forgotten metal stent while the other case reports had plastic stents [1, 4, 5]. Whether this is contributory to the burden and extent of stones involvement is unknown.
Endoscopic sphincterotomy and stone extraction as a treatment modality for CBD stones clearance is successful in 80–90% of cases [5, 6]. There is very little information in the literature regarding forgotten biliary stents except for a few case reports [1, 4, 5]. Some of these cases fail endoscopic management necessitating open surgery [1, 4]. This was the case with our patient. The largest case series of five patients was reported by Odabasi and colleagues [5]. In their case series, two patients were managed with cholecystectomy + CBD exploration + T-tube, one successfully managed with ERCP, one with Hepaticojejunostomy and the other with Choledochoduodenostomy.
Endoscopic management has revolutionized biliary stones management in a big way. However, this management modality often fails in forgotten stents necessitating open surgery. Forgotten stents can cause serious complications. We recommend the development of stent follow-up electronic registries with patient contact details, scheduling and reminder functionality to facilitate identification and tracking of patients lost to follow-up. Importance of education of patients and their next of kin about the implications of noncompliance to follow-up is emphasized.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONFLICT OF INTEREST
None declared.
REFERENCES
- stents
- cholangitis
- choledocholithiasis
- drug clearance
- endoscopic retrograde cholangiopancreatography
- bile fluid
- calculi
- common bile duct
- differential diagnosis
- follow-up
- metallic stents
- surgical history
- cholecystectomy, open
- roux-en-y hepaticojejunostomy
- plastic stent
- lost to follow-up
- mammary duct exploration
- cholelithiasis



