-
PDF
- Split View
-
Views
-
Cite
Cite
Awrad Nasralla, Bonnie Tsang, Unusual osseous metaplasia following hernia repair with Prolene mesh: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz251, https://doi.org/10.1093/jscr/rjz251
Close - Share Icon Share
ABSTRACT
The use of Prolene mesh for repair of various hernias is very common. As with any surgical procedure, it can be associated with complications such as seroma, hematoma and wound infection. However, it is uncommon to develop heterotopic ossification following incisional hernia repair with Prolene mesh. Herein, we report a case with chronic abdominal pain secondary to heterotopic ossification occurring after incisional hernia repair with Prolene mesh. It is crucial to report uncommon reactions to the mesh in order to aid in diagnosis of unexplained abdominal pain post hernia repair, after common etiologies are ruled out.
INTRODUCTION
Incisional hernia repair with mesh is one of the most common surgeries performed worldwide. It is estimated that 20 million hernia repairs are performed annually [1, 2]. Although the use of mesh reduces the recurrence rate of hernia repairs, it is associated with complications including seroma, hematoma, wound infection, chronic pain, calcification, erosion causing fistula formation and small bowel obstruction secondary to adhesions [2]. We present an unusual case of osseous metaplasia following incisional hernia repair with Prolene mesh.
CASE REPORT
A 65 year-old male was suffering from chronic abdominal pain and foreign body sensation following incisional hernia repair with mesh in 2010. In March 2010, the patient underwent an open right hemicolectomy for benign multiple colonic polyps and subsequently developed an incisional hernia. In November 2010, he underwent open incisional hernia repair with an onlay Prolene mesh. Subsequent to the mesh repair, he had sharp pain in the epigastric area particularly when bending forward and fullness in his upper abdominal region. He was referred to the outpatient general surgery clinic at a tertiary level hospital for an assessment. On focused abdominal exam, he had a midline laparotomy incision with no acute signs of infection. There was fullness superior to his umbilicus with a palpable subcutaneous mass measuring approximately 6 cm in diameter. Cross sectional imaging revealed an ovoid collection in the anterior abdominal wall, measuring 4.4 × 8 cm on magnetic resonance imaging (MRI) and 3.3 × 5.4 cm on computed tomography (CT). In addition, an abnormal calcification superior to the collection could be appreciated on CT (Fig. 1). These findings were suggestive of a chronic hematoma and scar tissue. The patient agreed to undergo debridement of chronic hematoma and partial mesh excision. Intraoperatively, the ovoid collection was approached via a midline incision and was encountered after dissection through the subcutaneous tissue. It was comprised of a thick rind of scar and fibrous tissue, measuring approximately 8 × 8 cm. It was unroofed, with immediate expression of old hematoma as well as fibrous tissue. Part of the overlying Prolene mesh and thick scar tissue were excised. The remainder of the Prolene mesh was well incorporated to his fascia and left in place. As the superior aspect of the collection was dissected out by entering deep to the fascia, a piece of calcified tissue was dissected out from the preperitoneal space superior to the mesh. It was suspected to be heterotopic ossification, and it was removed (Fig. 2). The fascia was then primarily repaired, and then the incision was closed in layers after thorough irrigation. On postoperative follow-ups in the clinic at 2 and 6 weeks, the patient was doing well, and his pain had improved significantly.
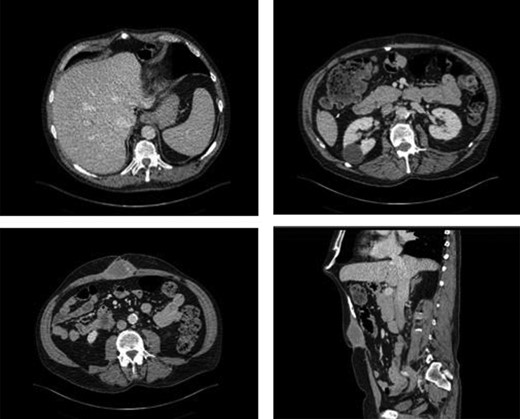
CT of the abdomen demonstrating anterior abdominal wall collection and the abnormal calcification. It revealed an ovoid collection within the anterior abdominal wall in the midline inferior to the mesh measuring 3.3 × 5.1 × 5.4 cm. In addition, it showed the abnormal calcification below the xiphoid process.
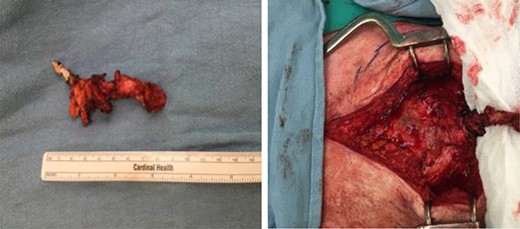
Intraoperative finding of the abnormal calcified tissue below the xiphoid process.
Symptoms of epigastric pain and fullness in the upper abdomen were gone. There was no recurrence of an incisional hernia on clinical examination.
Specimen sent for microbiology was negative for fungal and bacterial growth. Histopathological examination of the specimen revealed soft tissue with osseous metaplasia which is consistent with heterotopic ossification. The cause of this patient pain was likely secondary to a chronic hematoma and scarring, and surprisingly, an abnormal calcified mass consistent with heterotopic ossification.
DISCUSSION
Heterotopic ossification is usually encountered following trauma and burn and is especially common in orthopedic surgeries involving hip arthroplasties [3–6]. Heterotopic ossification after laparotomy is unusual. Since the first described case in 1901 by Askanazy, over 100 cases have been reported [7]. Since most patients remain asymptomatic, the true incidence is hard to determine. In a retrospective study, Kim et al. found evidence of heterotopic ossification on CT in approximately 25% of the studied patients following laparotomy [8]. However, only two of their cases were proven on histopathology.
Heterotopic ossification in the abdominal wall is associated with vertical laparotomy incisions and can develop in any layer of the abdominal wall from the subcutaneous tissue to the peritoneum [9]. It is by far more common in men than women [10]. There is only one other case of heterotopic ossification following hernia repair with Prolene mesh [7]. It involved a patient who underwent laparotomy for perforated peptic ulcer and presented 17 years later with acute abdominal pain secondary to fractured heterotopic ossifications, requiring excision of the bony material. Other cases of abdominal wall heterotopic ossification have described a time frame of presentation from weeks to years after the initial laparotomy.
The etiology of heterotopic ossification after laparotomy is unclear. One theory suggests that the disruption of the xiphoid process in a laparotomy involving an upper midline incision liberates periosteal cells, allowing these cells to implant along the vertical incision and later turn into mature bony tissue [9]. An alternate theory postulates that pluripotent mesenchymal cells in the linea alba undergo metaplasia, transform into osteoblasts and subsequently form bony deposition. This hypothesis, however, does not explain why heterotopic ossification only occurs in vertical incisions. Another theory suggests that heterotopic ossification may be related to the tension from sutures in fascial closure [10]. Perhaps the tension from the Prolene mesh repair in our case triggered bone formation and propagation. The mesh could also have served as a matrix for bone deposition.
The most common complications after abdominal wall hernia repair with mesh are seroma and/or hematoma formation, superficial and deep wound infection, hernia recurrence and mesh-related complications. In a patient with chronic pain after a hernia repair, after ruling out the common differential diagnoses, the possibility of heterotopic ossification should be kept in mind. Careful review of cross sectional imaging will reveal abnormal deposition of calcification in the abdominal wall. If the patient’s symptoms correlate with findings on imaging, surgical excision of the suspected heterotopic ossification should be considered.
Conflict of Interest
None declared.



